Numerous studies over more than two decades have demonstrated a robust relationship between climate and the dynamics of human diseases, such as cholera, malaria and dengue. Changes in climate, including both long-term warming trends and short-term climate variability, might affect patterns of disease. Xavier Rodó, a computational ecologist and climate dynamics specialist at the Barcelona Institute for Global Health and the Catalan Institution for Research and Advanced Studies in Spain, spoke to Nature about how climate modelling could be used to help prepare for future disease outbreaks—and the obstacles he has faced in implementing such systems.
How does climate affect disease transmission?
Climate impacts the emergence and spread of disease in myriad ways. Some are quite complex. Climatic conditions can have cascading effects on ecosystems that affect the likelihood of zoonotic spillovers, in which pathogens jump from an animal host to humans. We see, for example, that changes in temperature in the Brazilian Atlantic Forest drive waves of yellow fever in howler monkeys (Alouatta species) that precede human epidemics in a predictable manner1.
As climate changes, so too will the spread and intensity of disease outbreaks. The effects will not be the same everywhere, but changes in temperature and rainfall are going to lead to huge changes in the distribution and dynamics of zoonotic and vector-borne diseases. We are already seeing record numbers of mosquitoes carrying West Nile virus in New York City, for example, when it is typically found farther west.
What evidence is there for climate change influencing disease outbreaks?
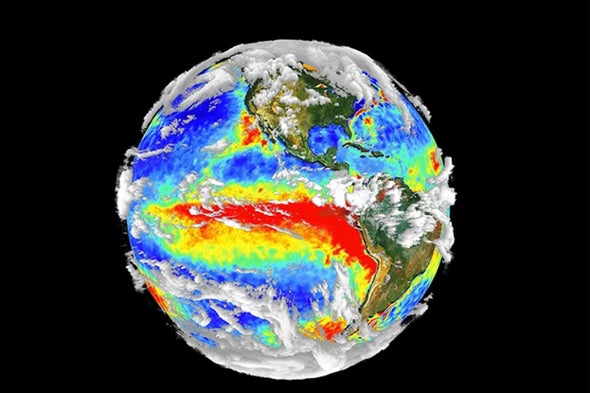
The first study2 I was part of that demonstrated this was published in 2002, in collaboration with Mercedes Pascual, a theoretical ecologist now at the University of Chicago, Illinois. In a previous study3, we had shown that the incidence of cholera in Bangladesh was affected by short-term climate patterns. Cases rose around six months after periods of increased local temperatures brought on by the El Niño Southern Oscillation (ENSO), a recurring climate pattern of warm (El Niño) and cool (La Niña) phases that occur irregularly every 3–7 years in the Pacific Ocean. But since the 1980s, there has been a marked intensification of ENSO, and we thought that this long-term trend might also be affecting cholera incidence. We looked at historical cholera data spanning a 70-year period, and saw that, between 1980 and 2001, incidence was strongly correlated with ENSO2. Data from a period before the intensification, however, showed no such correlation. The long-term trend of ENSO intensification, driven by a warming climate, seems to be affecting cholera dynamics.
.png)
How might climate modelling be used to predict and prepare for disease outbreaks?
With current tools, it is possible, in some regions, to forecast climatic conditions in the next season, the next summer or even further into the future—some El Niño events can be predicted up to two years in advance. Knowing months ahead of time that there is going to be an anomalous rainy season in a country, and how that is likely to affect disease incidence, makes it possible for public-health authorities to anticipate and plan their response. For example, they could stock up on medicines, or spray insecticides in certain areas to limit the hatching of mosquitoes.
What are the obstacles to developing these predictive models?
Both climate change and infectious-disease epidemiology are complex systems, and we need to bring together scientists from these very different disciplines to work on this problem. Right now, interdisciplinarity is spoken about more than it is seen. We also face difficulty attracting funding for projects of this kind, and opportunities to publish in established journals can be limited.
Availability of epidemiological data with which we can train and test our models is also a problem. For cholera, we have better historical data than we have recent data. It is similar for COVID-19—reporting has dropped off, so we have much better data for the first two years of the pandemic than we do for now. We need to understand that long-term data collection is fundamental if we want to be prepared for future threats.
What is the state of the development and implementation of such tools?
I have worked with an international team to develop a model that uses El Niño predictions to forecast dengue outbreaks in Ecuador. The model correctly predicted that in 2016, warmer temperatures and excess rainfall would lead to an outbreak in the city of Machala in March—three months earlier than would be expected. It also predicted that there was a 90% chance that incidence would exceed the average for the previous five years, and that a weak El Niño in 2019 would result in a low probability of a dengue outbreak during the typical peak season4,5.
This model and others have been adapted for use in other regions6. But these models have not yet been picked up by public-health authorities. People say they are interesting, but they don’t see the immediate economic benefit—unfortunately, saving lives is not valued as it should be. We have tried many times to implement our cholera prediction model in India and Bangladesh—Pascual more times than me—without success. I’ve also tried to set up a malaria forecast service in Madagascar, Senegal and Ethiopia, because there is a wealth of data the model can rely on there7. But we have been unable to convince the stakeholders.
This article is part of Nature Outlook: Pandemic Preparedness, an editorially independent supplement produced with the financial support of third parties. About this content.
References
-
Rodó, X. et al. Nature Med. 27, 576–579 (2021).
-
Rodó, X. et al. Proc. Natl Acad. Sci. USA 99, 12901–12906 (2002).
-
Pascual, M. et al. Science 289, 1766–1769 (2000).
-
Lowe, R. et al. Lancet Planet. Health 1, e142–e151 (2017).
-
Petrova, D. et al. Int. J. Climatol. 41, 3813–3823 (2021).
-
Lowe, R. et al. eLife 5, e11285 (2016).
-
Laneri, K. et al. Proc. Natl Acad. Sci. USA 112, 8786–8791 (2015).