When Robb Willer looks back on the early days of the COVID-19 pandemic—when leaders still had a chance to stop the virus from bringing the world to a halt—there’s a fateful moment that stands out. In February 2020, global health authorities spoke in one voice, advising the public not to wear masks to prevent infection.
“Seriously people—STOP BUYING MASKS!”, tweeted the then US surgeon general Jerome Adams, stressing that masks would not protect the general public from the virus. The World Health Organization (WHO) similarly advised that masks should only be used by health-care workers or people with a cough or fever.
But the message was soon reversed. Scientists knew that masks helped to prevent airborne viral infections; the early mask guidance was mainly geared towards preserving supplies for health workers. Once people realized that the authorities had not acted in their best interest, resentment began to smoulder.
The mask-messaging fiasco “was a big credibility mistake”, says Willer, a sociologist at Stanford University in California. “It hurt the response that they weren’t honest.” Leaders should always be transparent about why pandemic health measures are being implemented, he says, even if some facts are tough to swallow.
Although COVID-19 isn’t yet in the rear-view mirror, policymakers are already discussing how its lessons should shape our response to future pandemic threats, including the current outbreak of monkeypox. A fresh flood of behavioural-science research supports their plans. This work lends insight into which policies and campaigns are most effective at convincing people to follow health guidance that helps to stop the spread of disease.
The messages that have the most influence are not always the ones that policymakers assume will work. Appeals to the empathy and responsibility of the public, delivered by people whom listeners trust, can work better than outright mandates. Offering rewards for vaccination might be less effective than simply issuing reminders. Timing is also crucial—what motivates people at one stage of a pandemic might be less effective later. And, as the mixed messaging around masks shows, honesty is a baseline requirement.
The process of refining public-health outreach should be under way well before the next pandemic hits, says Matthew Goldberg at Yale University in New Haven, Connecticut, whose research focuses on persuasion. “We need to be doing the work now,” he says, “so that when the time arises, people can act quickly.”

Make it easy
To help society mount a collective defence against pathogens, researchers say that leaders should enlist human-behaviour specialists to play a much bigger part in health policy. This has been the Achilles heel of governments during the COVID-19 pandemic, says Armand Balboni, an infectious-disease researcher and chief executive of pharmaceutical firm Appili Therapeutics in Halifax, Canada. “Social scientists, anthropologists and psychologists were not used nearly enough,” Balboni says.
Part of crafting effective public-health messages is finding ways to avoid restricting people’s choices outright. Although health-related mandates are sometimes necessary during a pandemic, they can provoke a backlash and complicate further efforts to stem the spread of disease. Some businesses, for example, have rebelled against enforced closures during the pandemic. Instead, behavioural economist Varun Gauri at the think tank the Brookings Institution in Washington DC, advocates for a ‘nudge’ strategy that makes doing the responsible thing require very little effort. “The one thing that’s close to universal in behavioural science is, we’re all lazy,” says Gauri.
Making it easier to do the right thing could be as simple as placing hand-sanitizer units in more-accessible locations. In one study1, this strategy boosted people’s compliance with hand-hygiene advice without the need for mandates. And a study2 by behavioural scientist Katy Milkman at the University of Pennsylvania, Philadelphia, suggests that repetition is a powerful nudge strategy. People were more likely to have a vaccination when researchers sent them reminders compared with a control group, confirming previous ideas that reiterating messages gets results.
Some persuasion strategies that make intuitive sense, however, do not seem to have the desired result. After the first COVID-19 vaccines were rolled out in the United States, local and state officials invested millions in the idea that waving money at people would convince them to get the jabs. Leaders tried straight cash incentives, whereby people collected a set sum for getting vaccinated, as well as lotteries, in which vaccinated people were entered into a draw to win a cash prize.
But the concept often flopped. One study3 that gauged the effectiveness of vaccine lotteries found that vaccination rates were not significantly higher in lottery states than in non-lottery ones. Guaranteed cash payouts were somewhat more likely to encourage vaccination, a meta-analysis showed4. Still, the evidence on incentive-based persuasion “is pretty disheartening in general”, Milkman says.
She is now studying a twist on the lottery strategy that might deliver more value for money—a regret lottery. This involves telling people that their name has been entered into a draw to win a large amount of money, but if their name is pulled from the hat and they have not been vaccinated then they will have to decline the reward. When Milkman and her team tried this in Philadelphia5, vaccine rates in the area increased slightly compared with those in other, similar areas that did not have a regret lottery. “The one data point we have looks promising,” Milkman says, but further research is needed to confirm the finding.
Our better nature
Although personal gain might not be a strong motivator, empathy could be. Encouraging feelings of empathy in people could make them more likely to choose to protect others during a pandemic. One group of researchers reported6 that people who watched a video of a 91-year-old man describing being unable to visit his sick wife because of the COVID-19 pandemic were more likely to want to practice physical distancing than people in a control group who were not shown the film. Emotional appeals, therefore, could nudge people towards adopting helpful behaviours.
Invoking empathy can work even in populations that are suspicious of pandemic control measures. In a survey7 of more than 6,000 people in the United States and Europe, researchers found that people opposed to vaccines were most likely to draw back from their stance when presented with appeals to protect the health of others. They were less moved by the messages noting that they personally stood to benefit from the jab. The researchers say that policymakers should therefore stress vaccines’ collective benefits, such as protecting others and keeping the economy humming. Most people don’t like to be told what to do, Balboni says. “What is really helpful is when you can get people to take ownership or responsibility—that by and through their behaviour, they can actually protect other people.”
Winning over the most sceptical in society also involves making sure they get accurate information. During the COVID-19 pandemic, disinformation played a major part in sowing division and undermining the authority of health officials, Gauri says. That paved the way for fast viral spread and low vaccination rates.
To keep fake news from gaining a foothold, Milkman says, health departments need to be transparent and honest when they communicate with the public. That doesn’t mean describing every aspect of a crisis in detail, but it does mean ensuring that the messaging at the heart of health campaigns is bulletproof. Leaders disregarded this principle when they told people that masks were not effective, and in turn people began to ignore official health communication. This allowed conspiracy theories an opportunity to slither in.
Behavioural researchers also want to give people the skills they need to better distinguish between bona fide health advice and conspiracy theory. Jon Roozenbeek, a psychologist at the University of Cambridge, UK, is testing a strategy of ‘immunizing’ people against disinformation by exposing them to controlled doses of it—just as a live-virus vaccine protects people from a full-blown infection. He has built this approach into a series of free video games. One of them, called Go Viral!, teaches people to be sceptical of pandemic fake news by playing at being outrageous disinformation czars, publishing false headlines such as “I was silenced for trying to speak out about unsafe coronavirus vaccine!”
After playing an inoculation game, people interpret fake-news tweets as less reliable than they did before, and they’re better able to spot deceptive tactics in a series of fake headlines8. “The robustness is quite good from a 15-minute intervention,” Roozenbeek says.
But preparing the public is only a start. To limit the toll of disinformation in future pandemics, Gauri thinks public-health authorities will need to take a bigger, legislative approach to the problem. “If you’ve got a good regulatory scheme in place to prevent it, that’s really crucial,” he says. That could mean, for example, creating transparency laws that require online platforms to inform users of the source of suspect health content, without promoting active censorship of that content.
A trusted voice
The source of health information is important not only for helping people to tell fact from fiction. One of the major insights that behavioural scientists gleaned from the 2014 Ebola epidemic in West Africa was that the messenger mattered even more than the message being conveyed. People were more comfortable following lifesaving recommendations and seeking Ebola treatment if local leaders, rather than Westerners, communicated health guidelines. “If you didn’t have spokespeople who were credible, respected, trusted authorities within the community, it didn’t really matter what the content of your message was,” Willer says. “If you’re an untrusted outsider, you can’t get anywhere.”
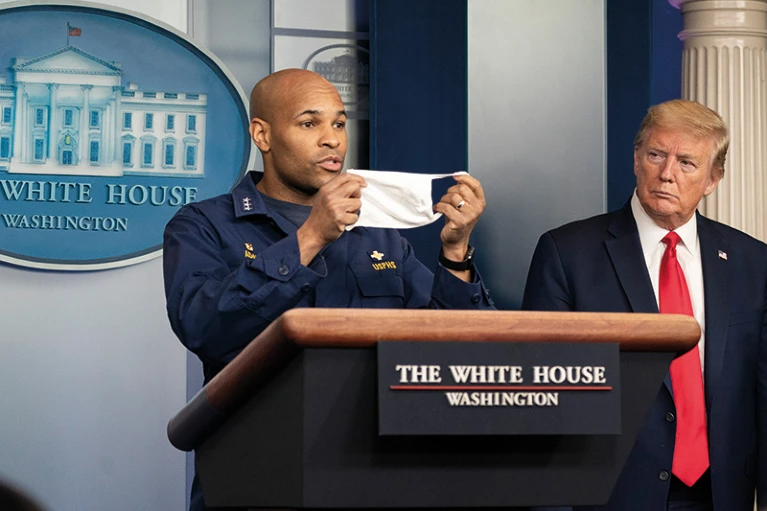
One team of researchers has memorably shown the lifesaving wallop a well-chosen pandemic messenger can pack9. The team culled footage of former US president Donald Trump urging people to have the COVID-19 vaccine, then wove the clips into a 27-second YouTube video. When the researchers aired the Trump message online in US counties with low vaccination rates, hundreds of thousands more people got vaccinated. “For the most opposed people,” Willer says, “he was arguably the most respected person in the world to tell them.”
In future pandemics, well-chosen pastors, community leaders or local influencers could be used more liberally to promote essential public-health messaging. Although some celebrities and sports stars did this during the COVID-19 pandemic, health authorities could reach out to a wider pool of candidates who have their own distinct followings. “If we can find those people early, or even pre-record them, that might be useful to have that ready to go when the time comes,” Gauri says.
The timing of public-health messaging is also important to its success—the earlier that health departments issue clear guidance on responding to a pandemic, the better. That’s because people are most open to persuasion when they first learn the facts about a situation, Willer says. “You want to jump on the critical windows when they appear.”
A study of the Italian population, which was among the hardest hit by the first waves of COVID-19, found that almost everyone believed public-health messaging during the early stages of the pandemic—even people who did not generally trust the government10. That high level of buy-in cleared the way for strict quarantine strategies that limited the pandemic’s spread.
But once people start to feel saturated with information, the power of public-health messaging can start to wane. When people received informational messages about how COVID-19 spreads, these messages decreased trips outside the home only for those who had started socially distancing in the past couple of weeks11. For those who had already been practising distancing for a month or more, the messages had almost no effect, and even decreased adherence to distancing guidelines.
Once people have been bombarded with messaging on a certain topic, “your message is going to struggle to have influence in that cacophony of voices”, Willer says. At that point, the best chance to impart the message has passed.
Preventive behaviour
Health officials have a long way to go to craft pandemic communications that prompt unified public action. The next-level goal—stimulating behaviour in advance of a pandemic that will reduce the chances of one erupting—might, therefore, seem unrealistic. But pre-emptive action is better than reactively attempting to tamp down global disease spread. And some researchers are asking whether behavioural science can be marshalled to help achieve that goal.
Because some pathogens can jump readily from wild animals to humans, coordinated public-health messaging about the importance of safe animal handling could be instrumental in heading off the next pandemic. Disease-detection platforms, such as the National Respiratory and Enteric Virus Surveillance System of the US Centers for Disease Control and Prevention (CDC), could also allow swift action to stave off pandemics.
But to get the public on board with following animal-handling guidance and responding to virus alerts early, leaders need to start promoting trust in health officials now, says Tom Kenyon, former director of the CDC’s Center for Global Health and chief executive of the global health non-profit organization Project HOPE in Washington DC.
To foster that outcome, Kenyon thinks that governments should allocate more funding to local public-health departments so that they can raise their profile in communities before the next lethal virus emerges. That way, he argues, residents will understand better how health departments work to protect people and will be more likely to heed official guidelines about how to prevent a pandemic from taking hold. “People know the police station, the fire station, the mayor’s office. They don’t know the health department,” Kenyon says. “The first thing is to demonstrate to the public what good public-health infrastructure does for them on a day-to-day basis.” Countries with low levels of COVID-19 spread are consistently those where people have high levels of trust in their governments and communities, researchers have reported12.
Reaching the levels of trust needed to stamp out pandemics will be a slog—and missteps over the past few months in response to the spread of monkeypox, such as mixed messaging about whether or not the virus is sexually transmitted, show that health departments have a long way to go. But researchers stress that better containment is possible—thanks to growing knowledge about how to promote coordinated public action. “It’s not hopeless,” Milkman says.
At the heart of improved preparedness efforts, Balboni says, should be the recognition that when leaders communicate clearly and honestly about the rationales behind pandemic policies, much of the public will respond. “When we can show people why it’s important that they change their behaviour—not just ‘Do it because I said so’—you actually start to push people in a direction that’s helpful.”
This article is part of Nature Outlook: Pandemic Preparedness, an editorially independent supplement produced with the financial support of third parties. About this content.
References
-
Cure, L. & Van Enk, R. Am. J. Infect. Control 43, 917–921 (2015).
-
Milkman, K. L. et al. Proc. Natl Acad. Sci. USA 118, e2101165118 (2021).
-
Law, A. C. et al. JAMA Intern Med. 182, 235–237 (2022).
-
Brewer, N. T. et al. Lancet Reg. Health Am. 8, 100205 (2022).
-
Milkman, K. L. et al. Nature Hum. Behav. https://doi.org/10.1038/s41562-022-01437-0 (2022).
-
Pfattheicher, S. et al. Psychol Sci. 31, 1363–1373 (2020).
-
Galasso, V. et al. NBER Working Paper 29741 https://doi.org/10.3386/w29741 (2022).
-
Basol, M., Roozenbeek, J. & van der Linden, S. J. Cogn. 3, 2 (2020).
-
Larsen, B. et al. NBER Working Paper 29896 https://doi.org/10.3386/w29896 (2022).
-
Barari, S. et al. Preprint at medRxiv https://doi.org/10.1101/2020.03.27.20042820 (2020).
-
Krpan, D. et al. Behav. Public Policy. 5, 153–179 (2021).
-
COVID-19 National Preparedness Collaborators Lancet 399, 1489–1512 (2022).


