In 2017 Ray Kaplan, a parasitologist and veterinarian then at the University of Georgia, started receiving e-mails from colleagues around the U.S. asking for help with resistant parasitic infections in dogs. The parasites were hookworms, a group of roundworm species that target animals and humans. Kaplan specializes in livestock animals, not pets. But the infections described in the e-mails sounded like cases of drug resistance, which he had studied in livestock parasites. The overuse of antiparasitic drugs in sheep and goats and the trade of these animals have led to widespread drug resistance across the globe. If drug-resistant parasites were spreading in dogs, too, that would be worrying. Kaplan had no idea just how big the problem was, however, until he started studying it.
Through a series of studies published over the past few years, Kaplan and his colleagues have traced the origin, evolution and spread of drug-resistant hookworms in dogs. Their findings implicate the greyhound racing industry in the rise of these superparasites. Once a national pastime, greyhound racing is now nearly extinct in the U.S. But it may have left a dangerous legacy that poses a risk to all dogs. The researchers' discoveries also offer a cautionary tale for the management of human parasite infections.
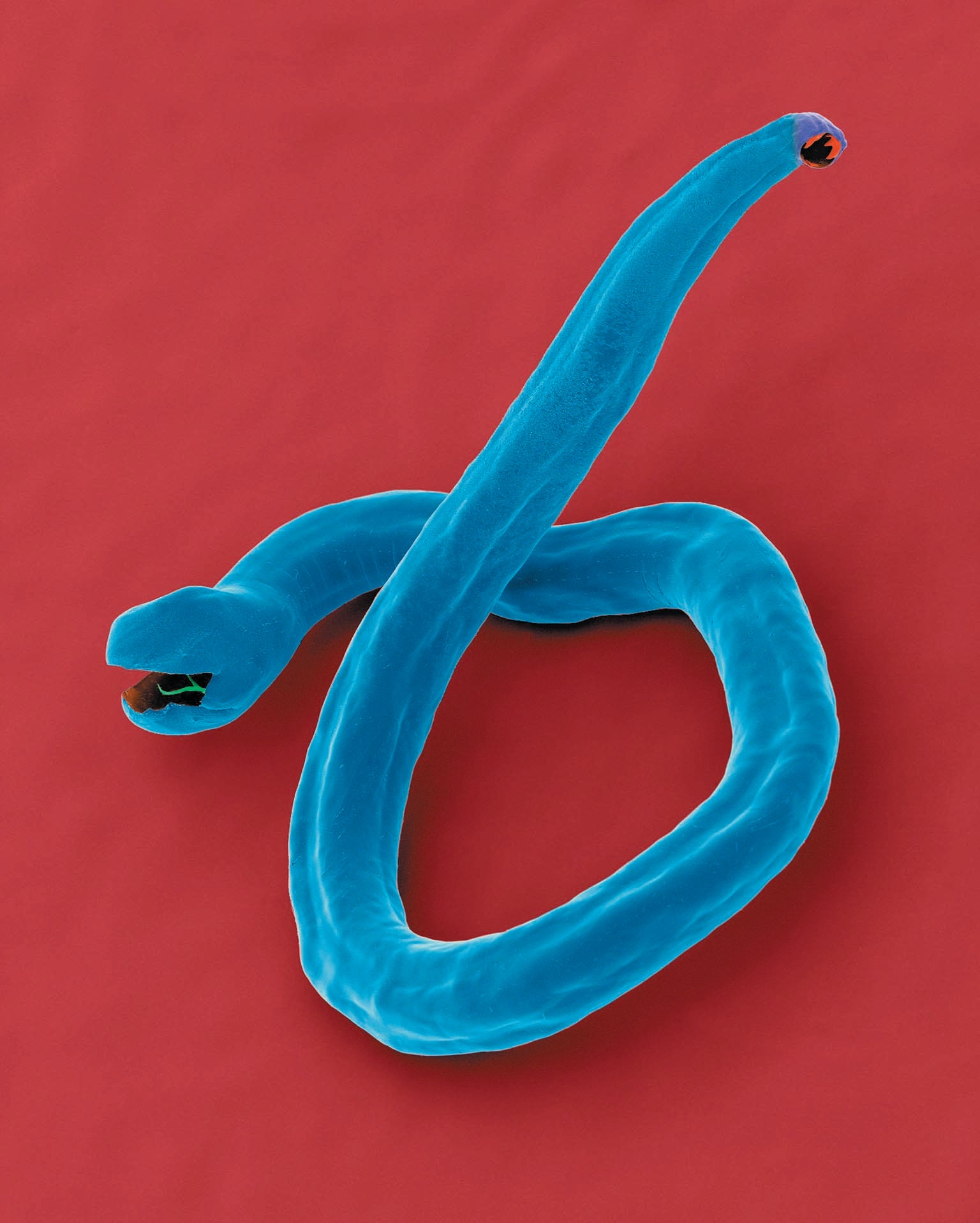
Parasitic roundworms are ubiquitous in the animal kingdom. Hookworms are named for their hook-shaped mouthparts, which they use to latch on to a host's intestinal wall and feed on its blood. In dogs, the most common species is Ancylostoma caninum. Adult hookworms live in the gut, and their eggs are spread through feces. Dogs can get infected when they come into contact with the larvae while walking or playing in contaminated areas or when they ingest larvae-ridden feces.
A. caninum infection is known by veterinarians to be potentially fatal for puppies. The worms consume so much blood that young animals can die from blood loss. A puppy is also at risk because high numbers of larvae can pass through the milk of its infected mother.
Hookworm is typically treated with one of three classes of antiparasitic drugs: benzimidazoles, macrocyclic lactones or tetrahydropyrimidines. To find out whether dog hookworms are resistant to any of these drugs, Kaplan began a series of laborious in vitro and in vivo tests on hookworm samples from three dogs with stubborn infections, including one greyhound named Worthy.
Greyhounds are notorious for developing resistant hookworm infections. For years veterinarians blamed this tendency on A. caninum's ability to lie dormant in its host's tissue and remerge after the original infection had cleared, a phenomenon known as larval leak. But Kaplan's initial results, published in 2019, showed that the worms in the three dogs he tested were resistant to all three main classes of drugs used to treat hookworm infections. Kaplan also tested for benzimidazole tolerance in worms from Worthy's housemate and from another retired greyhound, both of whom had histories of stubborn infections, and found that they were resistant.
These findings, along with the greyhound's hookworm reputation, led Kaplan to suspect something was happening on greyhound farms. What he found on further investigation was the perfect combination of factors to promote the evolution of drug resistance.
In the early 1990s greyhound racing in the U.S. was at its peak. In 1993 greyhounds were competing at dozens of tracks throughout 19 states, and the National Greyhound Association reported that 39,139 new dogs were born on greyhound farms that year. The sport began to decline in the early 2000s because of pressure from animal welfare organizations and the decision by many states to ban it. By 2020 the number of new greyhounds born on farms had dropped to 4,898 a year. Today dog racing is illegal in 42 states, and just two tracks remain active, although roughly 100 breeding farms are still operating.
During their heyday greyhound farms raised hundreds of dogs at a time and treated them regularly with dewormers—regardless of whether they had an active infection—to keep them in peak health. “That's exactly what you don't want to do if you want to avoid resistance,” says hookworm expert John Hawdon of George Washington University, who independently reported drug-resistant hookworms in another former racing greyhound in 2019.
Constant drug exposure means any worms that survive have a reproductive advantage and dominate the next generation. Moreover, the exercise pens for these dogs are set up on sand or dirt, which can be the perfect habitat for developing hookworm larvae. After dogs defecate in the pens, the hookworm eggs hatch, and the larvae eventually molt, reaching their infective stage within five to 10 days. Thus, every day when the greyhounds go out to run, they are exposed to resistant hookworm larvae from other dogs, and they seed the environment with resistant hookworms of their own.
(Veterinarians are encountering a similar but less severe situation with canine heartworm. Pet dogs typically receive regular preventive treatments for this parasite. Although drug resistance has been detected in these worms in some regions of the southern U.S., there are still effective treatments, and the resistance trait does not appear to have spread, probably because of differences in the biology and epidemiology of this parasite compared with hookworms. Kaplan says owners should keep their dogs on heartworm prevention and get a yearly test.)
To confirm that hookworm drug resistance was originating on greyhound farms, Kaplan carried out a second study, published in 2021, in which he sampled worms from two greyhound adoption kennels in Birmingham, Ala., and Dallas, Tex., and an active racing kennel in Sanford, Fla., and tested them for resistance. Samples from the Florida kennel were collected from the ground, making it impossible to know which dog they came from. But dogs at this kennel came from facilities in four other states—Colorado, Arkansas, Oklahoma and West Virginia—meaning any worms testing positive as resistant may be present in those locations as well. The results replicated what Kaplan had found two years earlier in Worthy: hookworms on the farms had high levels of resistance to all three drug classes. Worms that are resistant to benzimidazoles have up to three known single-nucleotide mutations in their DNA that confer resistance. These changes, each to one DNA building block, occur at three locations in the sequence of a single gene, making it possible to quickly screen worms' DNA and find out whether they are resistant to benzimidazoles. In the 2021 study of greyhound farms, 99 percent of the samples sequenced had one of the three resistance mutations.
The presence of drug-resistant hookworms at greyhound farms, Kaplan realized, poses a threat to the pet population. As the racing industry began its decline in the early 2000s, organizations sprang up to rehome the dogs, leading to thousands of greyhounds being adopted across the country in the past two decades. Greyhounds infected with drug-resistant hookworm could pass the parasites to other pet dogs.
Traditionally vets didn't pay much attention to hookworm infections in dogs, because there weren't that many cases. When doctors did see them, they prescribed drugs, but little follow-up occurred, and persistent infections were blamed on larval leak.
Then dog parks started gaining in popularity. Between 2009 and 2019 the number of such parks in the 100 largest U.S. cities increased by 74 percent. These spaces provide the perfect environment for the spread of parasites. As many as 500,000 hookworm eggs can be left in a single dropping from an adult canine, and once eggs and larvae are present in a park, it is nearly impossible to get rid of them. Two studies from 2020 and 2021 found that dogs visiting dog parks had a 70 percent higher prevalence of hookworm infections compared with the overall population.
Having established that greyhound farms were generating drug-resistant hookworms and that at least some pet dogs were infected with them, Kaplan needed a way to determine just how common the superparasites had become in the general dog population. He teamed up with John Gilleard and his laboratory at the University of Calgary in Canada. Gilleard has successfully adapted a DNA-sequencing technique that can screen hundreds of hookworm eggs from a single dog simultaneously for resistance mutations.
After sequencing fecal samples known to contain hookworms procured from diagnostic labs in Tennessee, Massachusetts, Illinois and California, the researchers were shocked. “We thought maybe 5 or 10 percent prevalence would be high,” Kaplan says. But to their astonishment, they found that one of the known resistance mutations was present in 49 percent of the fecal samples, and a novel mutation, which they confirmed also conferred resistance, was present in 31 percent. These results, published in March in PLOS Pathogens, suggest that roughly 50 percent of dogs in the U.S. with hookworm infections are carrying worms resistant to benzimidazole drugs. Although genetic screens for drug resistance are not possible for the other drug classes, Kaplan thinks it is likely that some of the worms will be resistant to them, too.

Just how big a problem drug-resistant parasites are depends on who gets infected. For most dogs, resistant hookworms are not fatal, and barring reinfection, the worms will eventually die. But the more these worms circulate in the population, the greater the risk of death for puppies and other vulnerable individuals.
A. caninum also can infect humans. The worms cause a painful condition called cutaneous larva migrans, in which larvae burrow in the skin and sometimes the eyes and wander around looking for the molecular cues that indicate they're in the right host. There are also rare cases of A. caninum causing severe gastrointestinal symptoms in humans, Hawdon says, a condition called eosinophilic enteritis. He noted some recent but unconfirmed reports of people with patent A. caninum infections, meaning reproductive adult parasites were detectable in their bodies, and points out that even if these particular cases remain unverified, “it is not inconceivable that it will happen in the future.” Because the same drug classes are used for hookworm infections in both dogs and humans, the rise of drug-resistant worms will complicate all treatment.
Although animal-to-human transmission of hookworm is generally considered uncommon, there are no reliable data on the number of cases in the U.S. Most reported infections in people are from travelers returning to the U.S. from tropical locations, particularly those where sanitation and animal husbandry conditions are poor. Zoonotic transmission may be underestimated, however. When Kaplan raised the issue of drug-resistant hookworm with the Centers for Disease Control and Prevention, he found little interest because cutaneous larva migrans is not something they monitor or track. But data from the other side of the world suggest there may be cause for concern: in 2020 researchers in Australia found that, contrary to prior belief, a hookworm species that commonly infects cats and dogs in Southeast Asia does infect people, too, and in some areas it accounts for up to 46 percent of hookworms found in humans.
Despite these worrying trends, Kaplan and Hawdon emphasize that we shouldn't blame the greyhounds. “It's a shame to stigmatize them because as the last of these tracks die, there's going to be even more of these dogs to adopt,” Hawdon says. Resistant worms are already circulating in the U.S. canine population, meaning all dogs can catch and spread them. Putting the risk to other dogs into perspective, Kaplan argues that although hookworms are present in most greyhounds, other breeds are the likely carriers when it comes to pet exposure. “There are only a few thousand greyhounds that are being adopted in a year,” he says. But “there are 100 million dogs in the U.S.,” and we know that the prevalence of the parasite in that population is about 4 percent.
Veterinarian Pablo David Jimenez Castro worked with Kaplan as a graduate student on the greyhound studies and is now co-chair of the American Association of Veterinary Parasitologists Hookworm Task Force. According to him, the best thing dog owners can do to protect their pets from hookworm, whether they adopt a greyhound or not, is to have their vet administer fecal egg tests for worms four times a year. If your dog has worms, be diligent with the treatment prescribed by the vet, and, most important, clean up after your pet. “Pick up the poop as soon as you can,” Jimenez Castro says. If owners prevent the infected dog from getting reinfected or passing the parasite to any other pets in the home, the worms will run their course and die. “[Dog owners] want to basically burn the backyard, the lawn, all of it just because they know that the dogs have hookworms,” Jimenez Castro says. But disposing of feces within 48 hours is enough to get any eggs they contain away from the area before they hatch and become infective.

Likewise, Jimenez Castro says, owners shouldn't be afraid of dog parks. “In big cities [such as] New York, the only place for a dog to be a dog is going to be the dog park,” he notes. But owners need to understand the risk and stay on top of checkups with the vet. Unfortunately, there is little that cities can do to eliminate hookworm in parks. Once larvae have made it to the grass and soil, they are impossible to find and kill.
In the meantime, researchers need to monitor other species for signs of infection with these superparasites. Our inability to treat the environment for worms means there is potential for wild canids that frequent urban spaces, such as coyotes and foxes, to pick up resistant worms as well. Wild canines range much farther than their domesticated counterparts and are not regularly treated or monitored for parasites, so they may be invisible spreaders of the resistant worms.
The rise of drug-resistant hookworm in dogs serves as a warning of what could happen with other species of roundworms that infect humans. Several serious, neglected tropical diseases in humans are caused by roundworms, including river blindness, lymphatic elephantiasis and ascariasis. Because these worms are genetically similar to dog hookworms and are treated with the same drugs, they can develop similar mutations that confer drug resistance. For the past decade public health officials, nongovernmental organizations and pharmaceutical companies have carried out mass drug administration programs in communities affected by the worms that cause these diseases. They have delivered millions of doses of antiparasitic drugs, mainly to children, who suffer the most from morbidity and developmental delays caused by heavy worm infections, with great success. Lymphatic elephantiasis was deemed eradicated in several countries after such programs were implemented.
Already there are reports of the same benzimidazole-resistance mutations appearing in human roundworms. Gilleard cautions that drugs alone cannot eliminate parasites, and, as the greyhound example shows, drug resistance can appear in one population and easily spread to others. Widespread surveillance for resistance—which is now possible with modern DNA sequencing technologies—is essential, he says. Without it, drug resistance will spread undetected before control programs can adapt, leading to a wormier world for everyone.


