Alzheimer’s disease has long been characterized primarily by the buildup of two proteins in the brain: beta-amyloid and tau. Decades of focus on beta-amyloid has failed to significantly help patients. So researchers are turning more attention to the second member of the duo.
“Amyloid hasn’t been as successful as we hoped,” says Jang-Ho Cha, an executive overseeing translational medicine work at pharmaceutical giant Novartis. “Tau has really emerged as a [potentially] more relevant target.”
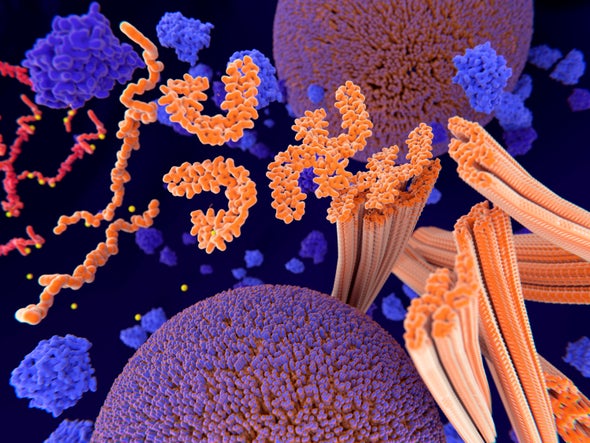
Tau was long thought to be a secondary actor. Amyloid plaque builds up first, largely outside of neurons, followed by tau tangles—filaments of the tau protein—which clog their insides. But research has found that people can continue to function well with amyloid in their brain. It is only when toxic tau starts to spread that people begin confusing “breakfast” with “baseball,” forgetting not just where they left their keys but how to use them.
Now scientists in labs across the world are trying to better understand the role of tau in neurodegenerative diseases and to figure out ways to track and tame it before brain cells—and families—suffer.
Normal tau helps assemble and maintain the structural scaffolding of brain cells. But various molecular changes can cause the protein to turn toxic and wreak havoc. Toxic tau misfolds like a shoelace tied in a mess of double knots instead of a neat bow. In this contorted state, tau appears to cause the misfolding of other tau proteins, which then clump together. “We think tau is an important target, certainly, in Alzheimer’s and potentially other diseases,” Cha says. “There’s certainly a lot of smoke around this fire.”
A study published in January in Science Translational Medicine showed that where tau builds up in a living brain predicts which areas of the organ will degenerate. This finding suggests that tracking tau over time is feasible and useful, says Anthony Fitzpatrick, an assistant professor of biochemistry and molecular biophysics and a principal investigator at Columbia University's Zuckerman Institute, who was not involved in researching the paper.
In Fitzpatrick’s own work, he uses an imaging technique called cryogenic electron microscopy (cryo-EM), which has 10 times the resolution of standard electron microscopy. His research shows that tau tangles form a distinctive shape that is always the same within a single patient and also varies in each of the several diseases it can cause. Alzheimer’s tangles look different from those in a patient with frontotemporal dementia. “Each tauopathy has a unique strain particular to each disease,” he says, noting that toxic tau is also involved in progressive supranuclear palsy, corticobasal degeneration and chronic traumatic encephalopathy, which affects football players and soldiers. Other neurodegenerative ailments, such as Parkinson’s disease, are associated with different toxic proteins.
But it is not yet clear whether these different tau shapes will matter, Fitzpatrick says. Any effective tau treatment may need to be delivered before these filaments develop their distinctive form, he and others say. Researchers are not sure whether an antibody designed to go after one type of tau will stop others as well.
The main problem in deciding which antitau strategy to adopt is that scientists do not yet understand the protein very well. Cryo-EM, for example, provides high-resolution images, but it captures brain tissues from cadavers. So researchers only know what tau filaments look like at the end stage of disease, not as they are beginning to clog brain cells, says Michel Goedert, a research group leader at the MRC Laboratory of Molecular Biology in England.
Researchers have only begun to understand what causes tau to turn toxic. A number of recent studies have suggested that the protein may take an aberrant turn after an inflammatory trigger, such as gum disease or an infection, or different conditions, such as “leaky gut,” in which microbes and other particles leak from the digestive system into the nervous system. George Tetz, a consultant at the Human Microbiology Institute, an independent nonprofit research organization in New York City, recently published a study showing that DNA can spur the seeding of toxic tau. “We strongly believe that the starting point for different neurodegenerative diseases is the appearance of certain bacterial DNA in the central nervous system,” he says.
If this theory proves true, it suggests there might be ways to stop the spark of an infection or another untoward event from igniting the raging fire of Alzheimer’s. But it is still very early days, Goedert notes, and more work needs to be done.
Another strategy—besides waylaying a toxic wrong turn—may be to figure out how to address tau buildup. Getting rid of the tangles might slow the progression of Alzheimer’s—or make things worse, explains Einar Sigurdsson, a professor in the departments of neuroscience and physiology and of psychiatry at the New York University Grossman School of Medicine.
There are now at least 20 compounds against tau in clinical trials, including nine antibodies and two vaccine candidates, Sigurdsson says. “No one knows if this is going to work yet,” he adds. So far, three antibody trials have been discontinued, and the companies have not been very forthcoming about the reasons, Sigurdsson says. He suspects that in two of the cases, the company was aiming at the wrong target: the drugs were designed to remove tau that is outside of neurons, he says, which is not a primary factor in the non-Alzheimer’s tauopathies that were being treated.
Attacking the tau tangles might actually be detrimental for brain cells, Sigurdsson says. The neurons that have tangles inside of them are still alive, while nearby neurons have been killed off. Targeting the tangle might kill these still functioning neurons, he explains. “If you want to clear the tangle, I think that you’re asking for trouble,” says Sigurdsson, who has spent the past two decades developing ways to go after toxic tau. A better approach, he says, would be to prevent the tau buildup from happening in the first place.
Another ongoing challenge has been figuring out how to tell whether toxic tau is present or whether its buildup is getting worse. If it is true that drugs are most effective when they reach the brain before much damage has been done, then early detection is crucial.
A relatively new scanning technology called tau positron-emission tomography (tau PET) can identify signs of tau tangles in the brain and potentially diagnose disease based on whether the protein can be detected and in what form. But Sigurdsson warns that the tau PET technology, not yet approved for clinical use, remains largely untested. The first-generation tau PET screens do not recognize the protein in all diseases that involve aggregated tau. New detection approaches being tested, using fragments of antibodies to bind to tau, have the potential to be even more specific, he says.
Goedert notes it is essential to find a reliable way to identify people most likely to get Alzheimer’s—through tau PET or the detection of some other biological marker. If, when he was 40 years old, someone had offered him a drug therapy that promised to prevent Alzheimer’s decades later, he probably would not have taken it, Goedert says. But if he had been told, at 40, that a biomarker indicated he was at high risk of eventually developing Alzheimer’s, he says he would have opted for the therapy. And preventing any neurodegenerative disease is likely to be easier than treating it. “I would argue that, in general, prevention is probably the way to go,” Goedert says. “Once people have symptoms, it may be too late.”
And even if there is a tau-based treatment, it may only be part of the answer, researchers agree. Combination therapy—perhaps attacking both amyloid and tau simultaneously—may be the only way to beat back Alzheimer’s once both tau filaments and beta-amyloid plaques have begun to accumulate, Sigurdsson says. The government has not allowed combination-drug trials so far—each drug has had to show some effectiveness on its own before it is allowed to be combined with another therapy. But Sigurdsson thinks that such combination approaches are likely to be needed and that trials will be permitted eventually. “That’s where we’re heading,” he says.
Despite the long list of failed therapies, Goedert says he remains optimistic that an effective treatment for Alzheimer’s will eventually be found. There are new ideas being tested—and there is always the chance that luck will strike, he says. Everything we know now, he notes, has been discovered in the last 35 years or so. What keeps him going, Goedert says, is the hope that his research will eventually benefit people with the disease—or prevent them from ever developing it at all. “The fact that nothing has worked well so far must mean that we don’t know enough,” he says.
Sigurdsson agrees that tau research will eventually pay off. “I’m optimistic that, with all these different targets that are out there, that we will have something, at least, that will slow progression—hopefully within the next 10 years,” he says.