By mid-December, the Northern Hemisphere is usually well into the start of its annual cold and flu season—but so far this year, even as the COVID-19 pandemic surges in dozens of countries, the levels of many common seasonal infections remain extremely low.
The pandemic caused by the SARS-CoV-2 coronavirus has infected at least 67 million people and killed 1.5 million worldwide. The patchwork of responses intended to fight the pandemic—from temporary lockdowns to mask wearing, social distancing, enhanced personal hygiene and reduced travel—has had a huge impact on other common respiratory illnesses, too.
In the Southern Hemisphere—now past its winter—seasonal influenza hardly struck at all. That looks as though it might happen in the north, too. Conversely, some common-cold viruses have thrived, and tantalizing evidence suggests that they might, in some cases, protect against COVID-19.
Despite humanity’s long history with colds and flu, the viruses that cause them still hold many mysteries. Scientists hope this year’s disrupted seasons could reveal new information about the transmission and behaviour of these unwelcome annual guests: how these viruses respond to health measures, how they interact and what that might mean for long-term disease burdens. “This is a natural experiment for so many respiratory viruses,” says Sonja Olsen, an epidemiologist at the National Center for Immunization and Respiratory Diseases, part of the US Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia.
The influenza fizzle
In May, at the tail end of the first wave of COVID-19 deaths in many nations, and when some of the strictest lockdowns were in place, health workers noted an abrupt and early halt to the 2019–20 flu season in the Northern Hemisphere.
That might partly have been an artefact caused by fewer people coming to a clinic for testing, experts say, but it was also attributable to the effectiveness of policies such as social distancing. After the pandemic started, positive tests for the flu virus plummeted by 98% in the United States, for example, whereas the number of samples submitted for testing dropped by only 61%. In the end, the US 2019–20 flu season was rated as ‘moderate’ by the CDC, which estimates that 38 million people fell ill with influenza, and 22,000 people died. That’s fewer than in recent years, but not unprecedented.
After the flu season in the north ended early, it hardly got going at all in the Southern Hemisphere. There were astonishingly few cases of seasonal flu there from April to July 2020—even as global COVID-19 cases continued to climb. In Australia, Chile and South Africa, a grand total of just 51 cases of flu were spotted in more than 83,000 tests. “We know it’s less transmissible than coronavirus, so it makes sense,” says Olsen, but the decline was still “greater than expected”. Influenza’s absence has been attributed to pandemic-response measures, but they don’t tell the whole story.
“Some South American countries haven’t done such a good job controlling COVID, but even there flu is low,” says virologist Richard Webby at St Jude’s hospital in Memphis, Tennessee. “I don’t think we can put it all down to mask wearing and social distancing.” He suspects that the dearth of international travel played a part. Flu typically travels around the world from one winter to another, while maintaining a lower year-round presence in the tropics. Although the mechanisms underlying this behaviour aren’t entirely clear, the movement of people clearly contributes.

Increased influenza vaccination might have contributed to the disappearance, too. Australia, for example, saw more than 7.3 million flu jabs administered by 20 May 2020, compared with 4.5 million by that date in 2019, and 3.5 million in 2018. It’s unclear if that trend will hold in the north.
Vaccination rates in the United States for seasonal flu have been trending upwards for years: slightly more than half of the US population over six months of age was vaccinated in 2019–20, up 2.6 percentage points from the previous year. But it is unclear whether Americans will be more or less inclined towards flu vaccinations this year, particularly given the tumultuous backdrop of the pandemic and the change in president.
Viral unknowns
Most experts are cautiously betting on a very mild flu season for the Northern Hemisphere this year. That would be good news on many fronts—in particular, it would help to alleviate the potential burden on the health system, from hospitals to testing centres, caused by simultaneous waves of flu and COVID-19. But surprises could be in store.
No one really knows, for example, why one nation, such as Australia, can be hit hard by influenza for several years while a neighbouring country, such as New Zealand, sees very low rates, says Webby. Even influenza’s seasonality isn’t entirely understood, nor exactly how it travels around the globe. “We don’t have a real good handle on why it’s a winter disease,” he says. Untangling lessons about flu from this year’s data will be interesting but difficult, Olsen says, because pandemic policies and compliance vary on the national, state and even neighbourhood level.
And the changing trends could have consequences. If this year’s flu season does fizzle out in the Northern Hemisphere, that could make it harder to predict the right strains to put in 2021’s flu vaccine. It could also have intriguing, longer-term consequences. Webby speculates that a low-flu season might kill off less-common variants of influenza. “A lot of different flus have been circulating in recent years. Are they all going to make it out of this or not?” he asks. “It’s possible that what this season will do is actually make the virological picture a lot simpler. That may be permanent, potentially.”
At the same time, Webby adds, the lack of viral competition in human hosts could conceivably open a door for new swine-flu variants in the future. “We get a handful of those every year, in the agricultural-fair season,” Webby says. “One of the things holding those viruses back a lot is natural immunity. If flu is low for a few seasons, that might leave a gap for swine viruses to have more impact.”
“I am sure that flu will come back with a vengeance at some stage in the future,” says Robert Ware, a clinical epidemiologist at Griffith University in Queensland, Australia, “but it might take a few years.”
Bucking the trend
Influenza viruses aren’t the only ones affected by pandemic-response measures. There are hundreds of viruses that cause respiratory symptoms similar to those of a common cold, from parainfluenza to metapneumovirus. And most of these viruses, too, seem to have been held at bay in the Southern Hemisphere’s winter.
In particular, researchers saw some abrupt declines in respiratory syncytial virus (RSV), a common virus that typically infects young children and can sometimes cause serious conditions such as pneumonia. There is no vaccine for RSV, and the virus causes about 5% of deaths in children under five around the world. In Western Australia, RSV in children declined by 98% (and flu by 99.4%) through their winter 2020, even though schools were open.
The RSV reprieve might be only temporary, though. Data from Australia’s most populous region, New South Wales (NSW), for example, show RSV detections climbing back up in October. And a build-up of susceptible, uninfected children might result in bigger waves of infection in future, some researchers warn.
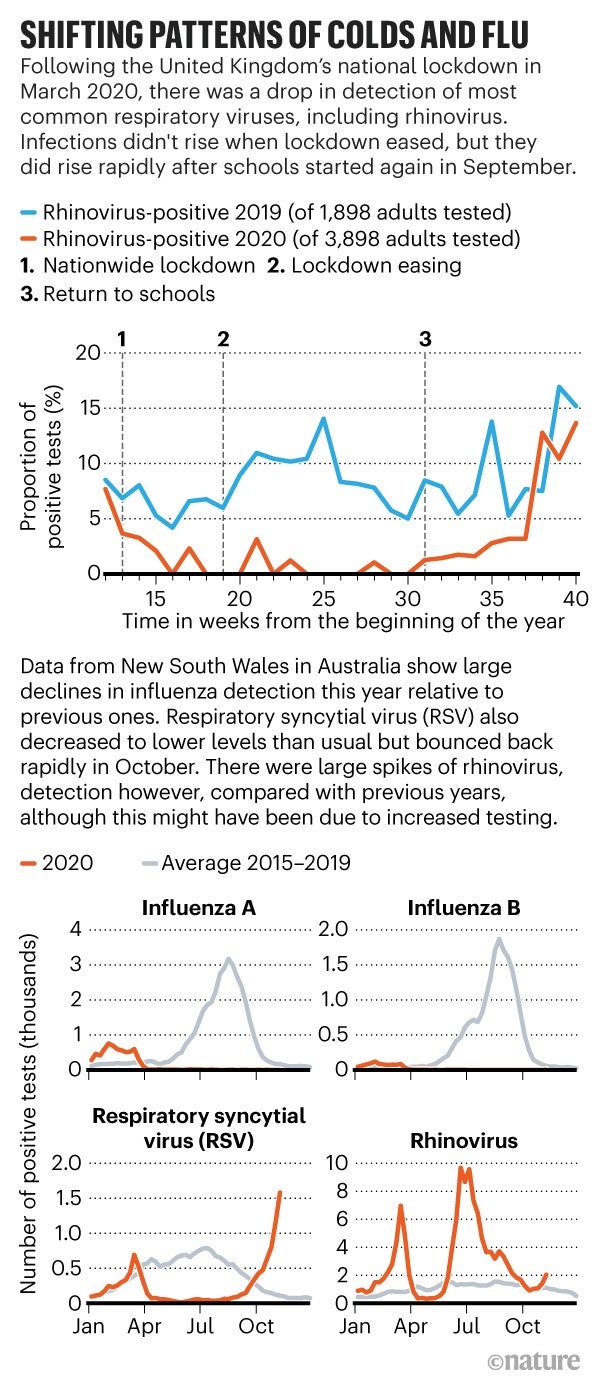
There is one major exception to the downward viral trend. “The one virus that’s not being halted is the rhinovirus,” says Janet Englund, a paediatric infectious disease researcher at Seattle Children’s Hospital in Washington. Rhinoviruses are the major cause of the common cold, especially in children. More than a hundred strains exist, and about a dozen typically circulate in any given community. In one study in Southampton, UK, rhinovirus detection in adults admitted to hospital remained lower over the summer of 2020 than in summer 2019, but shot up as usual once schools reopened in September. Data from NSW likewise show an apparent surge in rhinoviruses over the southern winter. Although some of these peaks are probably due to an increase in testing in people with mild cold symptoms, these viruses certainly did not decline as others did.
“No one really knows why” rhinoviruses are proving so persistent, says Englund. Some viruses that cause cold-like symptoms are very different from each other in structure; in particular, rhinoviruses, unlike influenza and coronaviruses, don’t have an outer lipid coat, or envelope, which is vulnerable to soaps and sanitizers. In NSW, detection of the non-enveloped adenoviruses, which also cause cold-like symptoms, held relatively steady throughout the southern winter, rather than crashing like flu or surging like rhinovirus. “The expectation is that rhinovirus is perhaps more stable on surfaces,” Englund says, allowing greater transmission between children on hands, desks and doorknobs. There is also thought to be greater asymptomatic transmission of rhinoviruses, which would allow them to circulate more freely in schools, even when sick children are staying at home.
The good news is that the common cold might help to protect people against COVID‑19. One study of more than 800,000 people, for example, showed that adults who had had cold symptoms within the previous year were less likely to test positive for SARS-CoV-2—although why this is so remains a mystery.
Cross-protection?
One possible explanation is that previous infection with a coronavirus (another cause of the common cold) could confer some immunity to SARS-CoV-2—although it’s notable that people can get the same coronavirus colds over and over again, and multiple cold viruses at once. Previous coronavirus infections do seem to generate T cells and B cells—immune-system cells that help to attack and remember pathogens—that can recognize SARS-CoV-2. These pre-existing cells might provide some partial cross-protection against the new coronavirus.
A few studies have shown that, because of other coronavirus infections, about one-quarter of people have antibodies that can bind to the SARS-CoV-2 virus, says Scott Hensley, a viral immunologist at the University of Pennsylvania in Philadelphia. One study showed that these antibodies can actually neutralize SARS-CoV-2 infections, stopping the virus from invading cells. Strong cross-neutralization of SARS-CoV-2 by antibodies against other coronaviruses would be “really spectacular”, says Qiuwei Abdullah Pan at Erasmus University Medical Center in Rotterdam, the Netherlands, because it would open the door to universal coronavirus vaccines that protect across the board. But other studies, including Hensley’s, found that these antibodies cannot neutralize SARS-CoV-2 or protect against COVID-19. “Cross-neutralization has not been proven,” says Pan. Even if it is, he says, “I would expect the activity would probably be very moderate.”
Another way that seasonal colds might be contributing to COVID-19 immunity is that a current rhinovirus infection might interfere directly with SARS-CoV-2—perhaps by kicking off interferon responses, part of the immune system that inhibits viral reproduction. A study by Ware and his colleagues, for example, shows that someone with a rhinovirus infection is 70% less likely to also get a common coronavirus infection, compared with someone who doesn’t have the sniffles. Clinical microbiologist Alberto Paniz Mondolfi at the Icahn School of Medicine at Mount Sinai, New York, and colleagues have shown markedly few rhinovirus co-infections in people with SARS-CoV-2 in New York City. “Rhinovirus is one tough virus,” says Paniz Mondolfi. Its fast growth stops other viruses from taking off, and it could conceivably be outcompeting SARS-CoV-2, he says.
This viral interference might be a powerful effect. Ellen Foxman, an immunologist at the Yale School of Medicine in New Haven, Connecticut, and colleagues have found evidence that rhinoviruses might have derailed the influenza H1N1 pandemic that occurred in 2009, for example. Hospitalized adults had fewer-than-expected instances of co-infection with both viruses. And, in cell cultures, rhinovirus infection stopped that strain of H1N1 from infecting cells. Foxman is now looking to see whether rhinovirus infection can block SARS-CoV-2; she expects results soon.
Overall, it’s a “very likely scenario” that rhinoviruses and other coronaviruses will help to stem the spread of COVID-19, says Paniz Mondolfi. “I think many virologists, like me, have been waiting for this season to look at how this will evolve.”
But with so many unknowns surrounding all these viruses, most researchers say that people should be ready for a worst-case scenario—from a bad flu season compounding the challenges of COVID-19, to future outbreaks of RSV. “It’s best to be prepared,” says Olsen. “We don’t know what’s going to happen.”
This article is reproduced with permission and was first published on December 15 2020.


