Seizures are like storms in the brain—sudden bursts of abnormal electrical activity that can cause disturbances in movement, behavior, feelings and awareness. For people with epilepsy, not knowing when their next seizure will hit can be psychologically debilitating. Clinicians have no way of telling people with epilepsy whether a seizure will likely happen five minutes from now, five weeks from now or five months from now, says Vikram Rao, a neurologist at the University of California, San Francisco. “That leaves people in a state of looming uncertainty.”
Despite the apparent unpredictability of seizures, they may not actually be random events. Hints of cyclical patterns associated with epilepsy date back to ancient times, when people believed seizures were tied to the waxing and waning of the moon. While this particular link has yet to be definitively proven, scientists have pinpointed patterns in seizure-associated brain activity. Studies have shown that seizures are more likely during specific periods in the day, indicating an association with sleep-wake cycles, or circadian rhythms.
In 2018 Rao and his colleagues reported the discovery of long-term seizure-associated brain rhythms—most commonly in the 20- to 30-day range—which they dubbed “multidien” (multiday) rhythms. By examining these rhythms in brain activity, the group has now demonstrated that seizures can be forecast 24 hours in advance—and in some patients, up to three days prior. Their findings, published on December 17 in the Lancet Neurology, raise the possibility of eventually providing epilepsy patients with seizure forecasts that could predict the likelihood that one will occur days in advance.
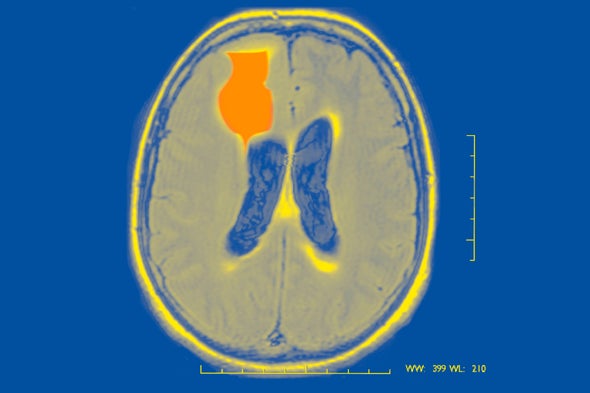
In their latest study, Rao’s group conducted a retrospective analysis of data collected during a nine-year clinical trial with participants who had a Food and Drug Administration–approved, implanted neurostimulation device, NeuroPace, which uses a type of electroencephalograph (EEG) to monitor both seizures and interictal epileptiform discharges—pathological spikes in brain activity that occur between seizures. (One of the study’s authors, Thomas Tcheng, is the senior director of preclinical research at NeuroPace.)
Using data about the timing of interictal epileptiform discharges and past seizures, the team developed a computational model that estimated whether or not a patient was at risk of a seizure in the subsequent hours or days. Maxime Baud, an epileptologist at the University of Bern in Switzerland and a co-author of the study, explains that the researchers were not trying to predict when, exactly, the next seizure will happen but rather to identify the probability that a seizure would happen over a given time period—akin to how weather forecasts provide a percentage of the likelihood of rain or shine on a given day.
When the researchers compared their forecasts to the actual occurrence of seizures in 18 participants, they found that in 15 of them (83 percent), the algorithm performed better than chance at predicting seizures 24 hours in advance. In two of the patients (11 percent), it was able to forecast seizures up to three days in advance. To further validate the model, the team applied it to another, larger data set with 157 participants—this time, assessing whether the algorithm could forecast self-reported seizures, which are the primary tool used for assessment in the clinic. The researchers found it could forecast seizures over 24 hours in 103 participants (66 percent) and up to three days ahead in 61 (39 percent). In general, chances of a seizure were highest during periods when both circadian and multidien cycles of brain activity were near their peak.
“Prior work has been mostly focused on forecasting seconds to minutes to a few hours ahead of time. This group has built on the work with multidien cycles to [introduce] a multiday predictor,” says Hitten Zaveri, a professor of computational neurophysiology at Yale University, who was not involved in the research. “[The study] has clearly been done very well, with good data and good observations.”
Forecasting on these longer horizons could provide significant benefit for people with epilepsy. One of the biggest advantages is that it could help rectify deficiencies of existing treatments, says Jacqueline French, chief medical and innovation officer at the Epilepsy Foundation and a professor of neurology at New York University, who was not involved in this study. The major issue with one of the main therapeutics used to prevent seizures, a class of drugs called benzodiazepines, is that if they are taken continuously, they lose their efficacy. (Long-term use can also lead to addiction.) Limiting their intake to days when people are at high risk for seizures could make them more effective, French says. Seizure forecasts may also improve the efficacy of devices such as NeuroPace, which monitors brain activity and delivers pulses of electricity when seizures are imminent to attempt to ward off the event, Rao notes.
For some people, however, seizure forecasts could prove more frustrating than helpful. “If I told you that tomorrow, there’s a 90 percent chance of rain, and you packed an umbrella, and it doesn’t rain, you might be upset that you had to pack an umbrella. Or conversely, you might be upset with me if I said there’s a 5 percent chance of rain tomorrow, and you go outside in shorts, and it rains,” Rao says. This dilemma is one of the reasons a prospective trial—in which participants are followed forward in time (rather than doing an analysis of previously collected data)—would be beneficial, Rao adds. Not only would such a study provide more robust evidence that seizure forecasting is indeed feasible, researchers would also be able to assess how participants actually use this information. Only one prospective study of a seizure advisory system has been conducted to date: the NeuroVista trial, which demonstrated that it was possible to predict the likelihood of seizures minutes in advance.
One key limitation of Rao and Baud’s forecasting technique is that it requires a brain implant to record neural activity. But Baud contends that the interictal epileptiform discharges used to generate these forecasts can be picked up with the less invasive measure of placing EEG electrodes just under the scalp (subscalp EEG). One of the next steps is to attempt to use this method to generate seizure forecasts as well.
Other groups are working on completely different measures to generate these kinds of seizure forecasts. Philippa Karoly, a research fellow at the University of Melbourne in Australia, and her colleagues have found evidence that multiday cycles in heart rate are also associated with seizure occurrence in patients. (These results have been posted onto medRxiv, a platform that hosts papers that have not yet been peer reviewed.) “We believe that we can measure these underlying biological cycles from not just the brain but also from the heart and from other aspects of physiology that are also affected by the same triggering factors that are driving the cycles in the brain,” Karoly says.
The promise of seizure forecasts could transform clinical practice. Still, key questions, such as why multiday cycles of brain activity exist in people with epilepsy, remain unsolved. Scientists speculate that fluctuating hormones may play a role—or that they may have something to do with the underlying disruptions in the brain associated with epilepsy. It is also possible that multiday rhythms, like circadian rhythms, are one aspect of how every brain functions. “That’s one very important question that has not been answered yet,” Baud says.