“Hello, what brings you here today?” a doctor asks a patient.
“I’m here for my checkup,” the patient responds.
“Great, let’s start with some routine screening questions to see whether you have any risk factors we need to talk about,” the doctor says. “Do you exercise regularly? Do you smoke? Do you consume drugs or alcohol? Do you eat a healthy diet? Do you have access to a firearm inside or outside of your household?”
“No, no, no, no, yes,” the patient answers.
“Okay, let’s talk about firearm safety,” the doctor says.
Sounds simple, right? But it really isn’t. For years doctors have considered gun violence to be a public health issue. Nevertheless, most health-care workers still do not talk to their patients about guns. In many settings, questions about firearm safety are taboo except in special cases such as those concerning people who are at risk of suicide, which accounts for roughly 60 percent of the nearly 40,000 gun deaths in the U.S. every year. Such targeted screening, however, can introduce bias and stigmatization, which hinders our ability to normalize conversations about firearm safety with our patients.
If we could figure out how to make such safety checks routine, the harm reduction could be significant—and we could provide policy makers with valuable insights into how to depolarize, depoliticize and humanize discussions surrounding the prevention of firearm injuries. After all, we in the health-care lane have a unique opportunity to use an approach that focuses solely on safety and injury prevention, without involving the Second Amendment. Such universal “we ask everyone” strategies—which can remove the pressure to decide who does and does not need screening—have been used successfully in public health approaches to other polarized issues such as substance use, sexually transmitted diseases and HIV.
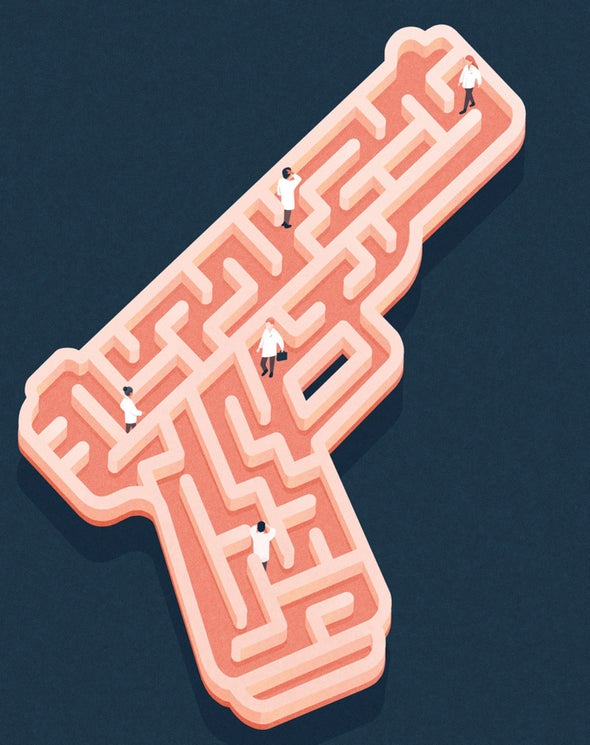
So why are many doctors hesitant to bring up firearm injury prevention? The truth is that we do not fully understand why. We know very little about how to normalize and humanize conversations about it—and gun-rights activists don’t want us to. A decade ago, for example, Florida went so far as to forbid physicians from asking patients routine gun-related questions (courts ultimately invalidated the law as a violation of doctors’ First Amendment rights). We do not have the data we need to inform us on the best way to have these talks. Health-care workers already face a number of evident barriers when it comes to such counseling, including a lack of education on the subject, fear of offending some patients, and inadequate resources for screening and counseling about preventive strategies.
Fortunately, the tide is changing. A combination of recent federal funding for research into firearm injury prevention, momentum in the health-care industry and the staggering level of gun violence in the U.S. might finally push doctors to ask every patient about firearm safety and gun violence risk during routine health visits. We need to work diligently with gun owners, survivors and community-based organizations alike to develop culturally competent education and intervention strategies geared toward making these talks a part of routine checkups.
Being able to ask the questions in the first place is an essential starting point. The country is at last getting behind concerned physicians in supporting a public health approach to gun violence prevention. If we succeed in depolarizing conversations about firearm deaths, as well as about the hundreds of nonfatal firearm injuries that happen every day in the U.S., it could have a ripple effect among the general public, further bolstering our argument that this matter is a public health issue.
Let’s make sure we get it right.