Lee Reeves always wanted to be a veterinarian. When he was in high school in the Washington, D.C., suburbs, he went to an animal hospital near his house on a busy Saturday morning to apply for a job. The receptionist said the doctor was too busy to talk. But Reeves was determined and waited. Three and a half hours later, after all the dogs and cats had been seen, the veterinarian emerged and asked Reeves what he could do for him.
Reeves, who has stuttered since he was three years old, had trouble answering. “I somehow struggled out the fact that I wanted the job and he asked me what my name was,” he says. “I couldn’t get my name out to save my life.” The vet finally reached for a piece of paper and had Reeves write down his name and add his phone number, but he said there was no job available. “I remember walking out of that clinic that morning thinking that essentially my life was over,” Reeves says. “Not only was I never going to become a veterinarian, but I couldn’t even get a job cleaning cages.”
More than 50 years have passed. Reeves, who is now 72, has gone on to become an effective national advocate for people with speech impairments, but the frustration and embarrassment of that day are still vivid. They are also emblematic of the complicated experience that is stuttering. Technically, stuttering is a disruption in the easy flow of speech, but the physical struggle and the emotional effects that often go with it have led observers to wrongly attribute the condition to defects of the tongue or voice box, problems with cognition, emotional trauma or nervousness, forcing left-handed children to become right-handed, and, most unfortunately, poor parenting. Freudian psychiatrists thought stuttering represented “oral-sadistic conflict,” whereas the behavioralists argued that labeling a child a stutterer would exacerbate the problem. Reeves’s parents were told to call no attention to his stutter—wait it out, and it would go away.
These myths and misconceptions have been debunked. Over the past 20 years, and especially in the past five to 10, a growing body of research has established that stuttering is biological in nature. Specifically, it looks like a neurodevelopmental disorder. In most of the more than 70 million people worldwide who stutter, the condition appears early in life, when children are learning to talk. Looking at the brains of people who stutter, scientists have uncovered subtle variations in both structure and function that affect the fluidity of speech. Compared with those who do not stutter, those who do have differences in neural connectivity, changes in how their speech and motor systems are integrated, and alterations in the activity of crucial neurotransmitters such as dopamine.
There is also a genetic component: researchers have identified four genes that dramatically increase the likelihood of this speech problem. Just as a flickering lightbulb is sometimes the result not of a bad filament but of faulty wiring throughout a room, these differences add up to what neuroscientists call “a system-level problem” in the brain.
These neurobiological revelations are already inspiring new treatments. A drug that targets dopamine overactivity is in a clinical trial, and others are in development. Several recent studies have shown benefits from brain stimulation. And given the importance of neuroplasticity in very young children, specialists now advise the opposite of a wait-and-see approach. “The brain findings affirm the idea that we want to get involved as early as we can,” says speech language pathologist J. Scott Yaruss of Michigan State University.
Some aspects of stuttering remain a puzzle. The condition affects about 1 percent of adults but roughly 5 percent of children, up to 80 percent of whom recover fluent speech. (So, yes, Reeves might well have outgrown it.) Scientists—and parents and therapists and, most dearly, people who stutter themselves—would like to know what accounts for the difference between persistent stuttering and recovery. Therapy can help but does not appear to explain it. Long-term studies of children may shed light on this, and such studies are just beginning to show results. And although a few genes linked to stuttering have been identified, their precise role in the disorder has not yet been pinned down.
But as more pieces fall into place, researchers and therapists hope the recognition of these biological causes will help to change society’s prejudices about stuttering. Although some people who stutter or have other speech impediments go on to accomplish great things—President Joe Biden struggled to get words out, as did the poet who recited at his inauguration earlier this year, Amanda Gorman—others have difficult lives. Many are underemployed and suffer from social anxiety and mood disorders. Psychiatrist and neuroscientist Gerald A. Maguire of the University of California, Riverside, School of Medicine stutters himself and has devoted his career to understanding the condition and developing pharmacological treatments for it. His brother, who also stuttered, died by suicide. “If we understand the biology, then we’re open to all sorts of treatments, and hopefully the stigma is less,” Maguire says.

From Pebbles to PET Scans
Stuttering has been recognized for thousands of years and exists in every language and culture. In addition to Biden, well-known people who have stuttered include Greek orator Demosthenes, who put pebbles in his mouth to practice speaking; King George VI of England, whose unconventional speech therapy was immortalized in the 2010 film The King’s Speech; and actor Samuel L. Jackson, who used curse words to improve his fluency. It is distinct from occasional or habitual word stumbles. Repeating words or peppering sentences with “um” or “ah” indicates hiccups in planning speech, whereas the underlying neurological differences in people who stutter disrupt a more basic level of speech production. “Everybody is dysfluent, but only some people stutter,” Yaruss says.
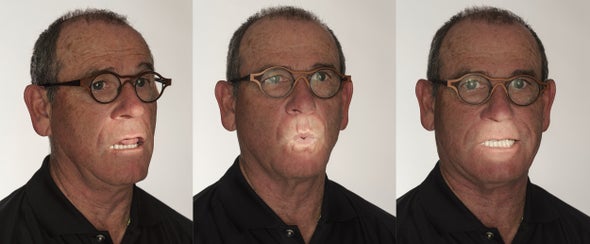
There are three types of stutters people experience: prolongations, stretching out a sound (mmmman); repetitions, in which syllables or sounds are repeated (my-my-my-myself); and blocks, in which the speaker initially cannot get any sound out at all. If a child continues to stutter past the age of about eight, they are likely to stutter throughout life.
Reeves describes the experience of stuttering as an unexpected loss of control. “You know what you want to say and how to say it—the words, the phrases, the sentence structure, the inflection—but all of a sudden you get stuck,” he explains. “You can’t move forward. You can’t move backward. All of the muscles are just locked.”
The first suggestion that stuttering might be neurological came in 1928. Samuel Orton and Lee Travis, a physician and speech language pathologist, respectively, theorized that stuttering was the result of competition between the brain’s two hemispheres. “They were on the right track,” Maguire says. But it took the arrival of sophisticated brain-imaging techniques in the 1990s to reveal neural differences in people who stutter. In 1995 Maguire and his colleagues published the first positron-emission tomography (PET) study of the problem, scanning the brains of four people who stutter, and reported consistent decreases in neural activity in language areas. Other small early studies found increased levels of dopamine in the striatum, a critical piece of the brain’s reward circuitry.
Building on this type of work, researchers tested antipsychotic drugs that block dopamine receptors and found the medications improved fluency in some people, although the drugs came with the risk of severe side effects such as parkinsonian movement disorders. Still, there were plenty of skeptics who were convinced stuttering had nothing to do with the brain. When Maguire presented his theory that stuttering was a brain disorder at a scientific conference in the late 1990s, he recalls, “I was kind of booed off the stage.”
The newest research uses high-tech scanners and advanced analytical techniques, and it proves these early researchers were onto something. In most people, language is predominantly supported in the left hemisphere. Adults who stutter show less activity in the left-hemisphere areas that support speech production and more activity in the right hemisphere than adults who do not stutter. For example, cognitive neuroscientist Kate Watkins of the University of Oxford identified an area in the left hemisphere close to speech regions, the ventral premotor cortex, that did not activate when people who stutter were speaking.
That area sits directly above an important white matter fiber tract linking auditory- and movement-control areas where Watkins and others have found structural differences in people who stutter. White matter is made up of axons, long neuronal projections that transmit impulses. “It’s all of the cables and wires that allow communication,” Watkins says.
That communication needs to be timed perfectly. To pull that off, axons are insulated with myelin, a fatty substance that speeds transmission. Well-myelinated axons in tracts usually run in the same direction, like the fibers in stalks of celery. But a kind of brain scan called diffusion-weighted imaging reveals that in people who stutter, the axons most likely crisscross.
Moreover, fluid and neurotransmitters should travel through white matter bundles much like water would flow through celery, along parallel fibers. In these brain scans, the flow is quantified in a measure called fractional anisotropy (FA)—the higher the FA, the more tightly organized the white matter. People who stutter have consistently lower FA values in this tract. Watkins suspects that means that brain areas the white matter was meant to feed sometimes are not getting the message and do not activate. (Parts of other white matter tracts in people who stutter, such as the corpus callosum that connects the cerebral hemispheres, show similar reductions in white matter integrity.)
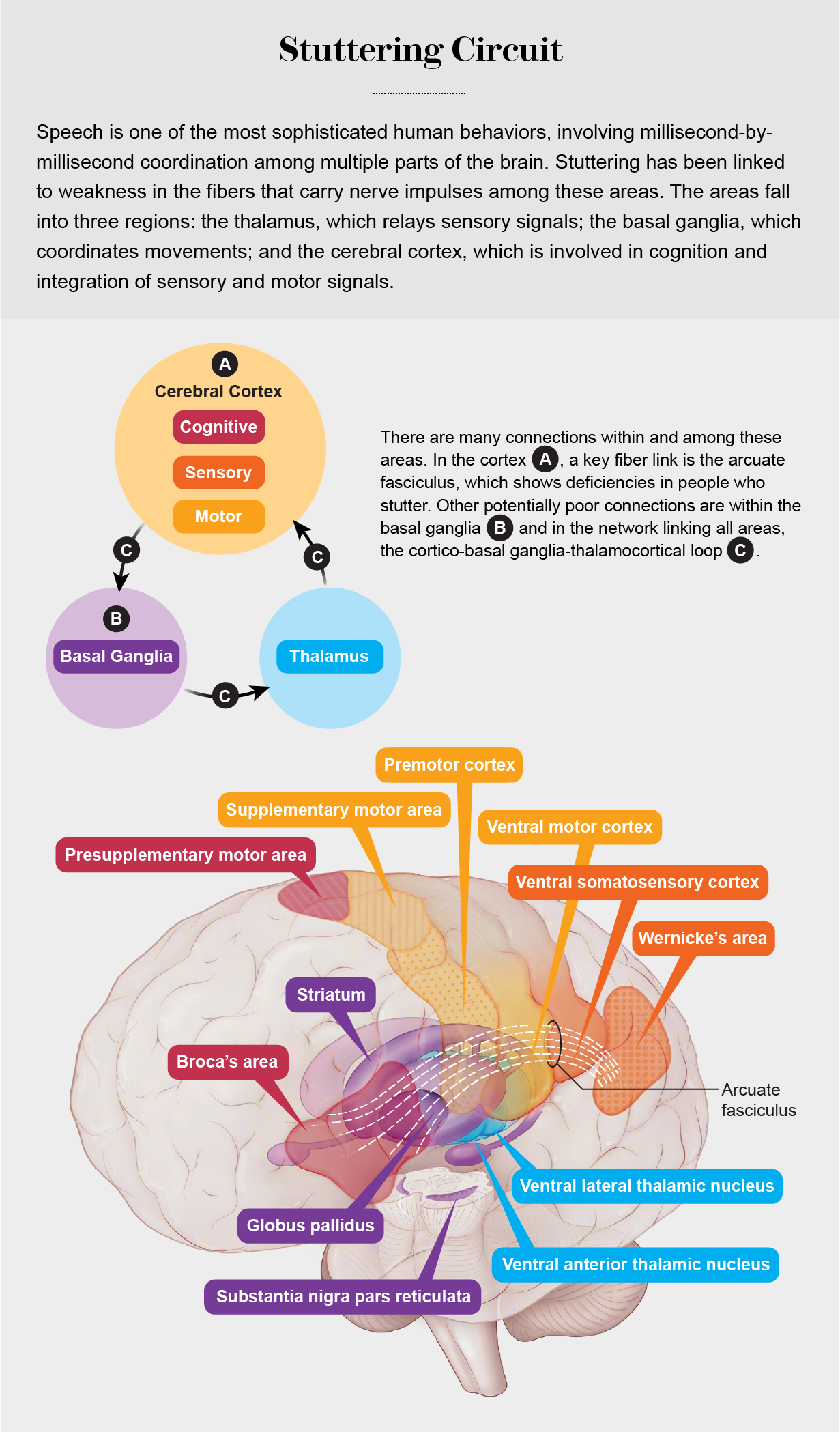
Functionally, people who stutter appear to have deficits in a brain circuit called the cortico-basal ganglia-thalamocortical loop, which also underlies auditory, speech and motor integration. As the name implies, the circuit connects structures deep in the brain—the basal ganglia, which includes the striatum, and the thalamus—with areas in the cortex closer to the brain’s surface. “Speech is one of the most complex motor behaviors we perform,” says neuroscientist Soo-Eun Chang of the University of Michigan. “It relies on millisecond coordination among neural circuits as well as muscles. Among other things, this loop supports smooth and timely initiation of movement patterns.”
It is not yet clear exactly why the breakdown occurs, but even subtle deficits could lead to difficulty producing fluent speech. “Everything’s pointing to the basal ganglia being the switchboard,” Maguire says. “If anything along that pathway is disturbed, it can lead to stuttering symptoms.”
Differences such as these could be at the root of stuttering. Or they could be compensatory changes, the effect of the brain trying to adapt to the experience of stuttering. Chang is trying to distinguish cause from effect by tracking more than 250 children beginning at the age of three and following them for at least four years. Some of the children recover from stuttering, and some do not.
In 2017 Chang and her colleagues reported that compared with children who did not stutter, children who did began with a weakness in white matter integrity in the left-hemisphere tract connecting auditory and motor regions. But in children who recover, white matter integrity became better organized over time. “That was increasing and normalizing in recovered kids, and it was completely plateaued or even going downward in persistent kids,” Chang says.
In both adults and children who stutter, she has found weakness on the left side of the brain. More consistently in adults so far, she has also discovered a pattern of overactivity on the right side, suggesting it is an adaptive, late-occurring change. The “million-dollar question,” Chang says, is whether there are detectable differences from the start between children who go on to recover and those whose stutters persist. “Having that objective marker early on would be critical,” she says, because it would indicate who is at greatest risk for continued stuttering.
All in the Family
Much of that risk is handed down with family DNA. Studies of twins and adopted children suggest genes explain anywhere between 42 and 85 percent of the risk of stuttering. Identical twins share a lot more genes than do fraternal twins, and in one study, 63 percent of identical twins both stuttered versus 19 percent of fraternal same-sex twins. The remaining risk may be caused by environmental factors (one indication of such nongenetic influence is that not every pair of identical twins both stutter), although some environmental factors can combine with genetic predisposition. Exactly what those environmental factors are is not known.
But some of the genes have been identified, thanks to work that geneticist Dennis Drayna of the National Institute on Deafness and Other Communication Disorders began some 20 years ago. Drayna traveled to Pakistan, where it is common to marry cousins, a practice that can strengthen the effects of genes within families. “It was easy to find great big families with lots and lots of cases of stuttering,” Drayna says.
In 2010 Drayna and his colleagues reported three stuttering genes: a mutation in GNPTAB, a gene that was previously identified in a severe genetic disorder entirely unrelated to stuttering, and mutations in genes called GNPTG and NAGPA. And then Drayna got an online question from a man in Cameroon asking about the prevalence of stuttering in his family—out of 71 individuals Drayna later met, 33 stuttered—and it led the geneticist to a fourth stuttering gene, AP4E1. (A report of a fifth gene is still unpublished.) Together those genes might at best account for 20 to 25 percent of cases, Drayna says. The high family prevalence of the problem indicates there are more genes to find, and to look for them, a consortium of 22 research groups led by Australian scientists is conducting a new genome-wide association study (GWAS) of people who stutter.
All the genes identified so far have to do with intracellular trafficking, or the transport of molecules within cells. In a 2019 study, Drayna and his colleagues found that mice carrying a mutation of the gene GNPTAB had abnormally long pauses in their vocalizations, similar to stuttering. And in those mice, they identified a deficit in astrocytes, a type of brain cell widely found in white matter tracts that interconnect the two cerebral hemispheres. It could be that mutations in lysosomal genes, which help to remove waste products, are one link between genetics and the neurology of stuttering.
Ending Stigma
The genetic origins of stuttering do not mean it cannot be treated. Already the newer research is informing therapy for stuttering. Pharmacological approaches are being fine-tuned. Maguire and his colleagues believe that medications that lower dopamine activity in certain brain circuits are the most promising approach to date. Antipsychotic drugs do just that. Maguire has successfully tested risperidone, olanzapine and lurasidone, all of which reduced the severity of stuttering, although none has received approval from the Food and Drug Administration. Unfortunately, these drugs can also cause unpleasant side effects such as weight gain and impaired movement. Still, some people, including Maguire, take them off-label.
Maguire is now leading a larger, randomized clinical trial of a drug called ecopipam, which is also being tested to treat Tourette’s syndrome. Ecopipam targets a different set of dopamine receptors than earlier drugs. In a small pilot study, the drug improved fluency and quality of life and had no significant side effects. But any pharmacological treatment for stuttering that wins fda approval is unlikely to work for everybody. “I think our next path will be personalized medicine, figuring out what’s really going on in [each] person,” Maguire says. “We’re learning now that stuttering is not going to be one condition.”
Brain stimulation with mild electric currents also appears promising. At Oxford, Watkins combined noninvasive transcranial stimulation with known speech-fluency strategies such as getting a group of people to read together in chorus or asking people to speak to the beat of a metronome. Such techniques have been shown to temporarily improve fluency in people who stutter, probably because they take advantage of external cues to initiate speech.
In a group who had combined treatment, Watkins found that the portion of their speech with repeated or prolonged syllables—or some other features of stuttering—dropped from 12 to 8 percent. But this percentage did not change in a control group who did not receive stimulation. Given the small size of the study and its short duration (five days), even that limited impact was enough to suggest they were on to something.
Adding brain stimulation to speech therapy may strengthen learning. “We were kind of consolidating that pathway, making it work more efficiently by stimulating it,” Watkins says. For now, many people who stutter have only traditional speech therapy to turn to, if they choose. The techniques usually involve practicing speech production but also learning to communicate effectively with a stutter. Speech therapy can be very effective but does not necessarily last—most people relapse at some point.
Partly in recognition of that fact and partly because of changing cultural awareness, the goal of therapy for people who stutter has shifted in recent years from trying to eradicate stuttering to trying to make it easier to accept and manage. “There’s a huge component that is coping-related,” Yaruss says. He likens it to learning to ice skate. The first time you strap on skates and go out on the ice, you’ll flail around and feel like you’re slipping or falling. But as you learn to tolerate that slipping feeling, you respond more expertly. “You can say, I know what to do when this happens; you move through a moment of stuttering more expertly.”
That shift in emphasis is a welcome one. Catherine Moroney, 54, is a physicist and software engineer at the NASA Jet Propulsion Laboratory. As a child, she says, “I basically couldn’t make myself understood.” Speech therapy greatly improved her fluency but only temporarily because she finished her therapy just as she was in the midst of a punishing physics degree program. Stress and anxiety do not cause stuttering, but they can make it worse.
Moroney, whose stutter is moderate now but used to be more severe, was fortunate to find a boss who cared only for the quality of her work, which involves studying clouds and their role in the climate system. She now takes the antipsychotic olanzapine off-label. “It just makes daily life a little bit easier.” But what really changed Moroney’s life was joining what she calls “my stuttering family.” “It may be counterintuitive, but the loudest and noisiest place in the world is a stuttering conference,” she says with a laugh. “Nobody ever shuts up. It is so freeing for those few days to be in the majority.”
Lee Reeves, a former chair of the board of the National Stuttering Association and an early advocate of the self-help movement in stuttering, agrees wholeheartedly. Speech therapy did improve his fluency, but the fact that his therapist was a clinical psychologist who addressed the mental stress of the condition was absolutely critical to his success. “I learned to stutter in a way that was acceptable to me,” he says.
Nor did his stutter stop him from becoming a veterinarian. Three weeks after he visited that animal hospital as a teenager, the vet—his name was Peter Malnati—called back and offered Reeves a job. Reeves worked for that clinic through the rest of high school and college and went on to a five-decade career as a small-animal vet, much of it in Plano, Tex. Now his days of frustration and embarrassment are long gone. “I still stutter. I stuttered yesterday, and I stuttered today,” Reeves says. “I hope I stutter tomorrow because it means I’m still alive.”