Michelle Boyer got an extra six years of life. Karen Koehler had six nearly symptom-free years, thinking she had beaten her diagnosis. And Doug Olson has officially been declared “cured” more than a decade after he thought he was out of options. These people are three of thousands who, in the past 10 years, have experienced both the promise and the challenges of an approach to treating cancer by manipulating the immune system. Instead of attacking cancer from the outside—slicing out tumors or dousing the body with toxic chemicals or radiation—immunotherapy energizes the complex and highly interactive cells and molecular signals of its defense networks to do the job from the inside.
Like those older approaches, immunotherapy has become one of the pillars of cancer care for blood cancers such as Olson’s and Koehler’s and for melanoma like Boyer had, as well as for bladder, breast and lung cancer—the last being America’s biggest cancer killer, responsible for more than 130,000 deaths in 2021.
The transformation has been dramatic, from just reaching oncologists’ radar a decade ago to beginning to catch on five to six years ago. “There has been a 180-degree change in the center of gravity in both cancer research and clinical oncology practice,” says Ira Mellman, vice president of cancer immunology at Genentech in California. Immunotherapy “has become the standard of care in lung cancer, which not long ago was treated with either surgery or chemotherapy, or both.” The results so far have been encouraging but far from universal, and progress has not been as fast as “a lot of us anticipated or hoped,” says Stanley Riddell, who researches immunotherapies at the Fred Hutchinson Cancer Research Center in Seattle. “Curing cancer’s not easy.” Given now to tens of thousands of patients, the treatments provide near miracles in some cases, dashed hopes in others.
Doctors are still at the beginning of understanding which patients will be helped by immunotherapy and which will not. Factors at play seem to include how many T cells have already made it into the tumor microenvironment, how hard it is for the immune system to recognize cancer cells, and even the patient’s makeup of gut microbes, Riddell says. Former President Jimmy Carter was almost 91 in August 2015 when he announced that his melanoma, the most lethal form of skin cancer, had spread to his liver and brain. News outlets readied their obituaries. But Carter received radiation and then an immunotherapy drug that releases the brakes cancer can put on the immune system, called checkpoint inhibitors. By December of that year, all evidence of his tumors was gone, and he has since celebrated his 97th birthday. It is likely that he saw such incredible benefits because his cancer resulted from years in the sun, which triggered a wide variety of mutations. That and damage from radiation made his cancer cells easier for his immune system to recognize once immunotherapy lifted the brakes.
Boyer, a Seattle resident, was diagnosed with advanced melanoma in her 20s, so her cancer was probably the product of fewer mutations. In 2013 she started a series of revolutionary treatments—some of which first became available in 2011—that prompted her immune system to identify, attack and shrink the tumors. But even unleashing the immune system was not enough to elicit a full-blown attack, and she died in 2019 at age 32.
Beyond the mutational burden of an individual’s cancer, doctors do not know much about who will or will not do well on these drugs. They have looked for years for molecular markers that could be predictive, but they have not had much success. While the hunt continues, researchers are testing drug combinations and other approaches, such as vaccinations, to stretch the benefits to more patients. Such combinations are needed both because cancers are complicated, being the product of various genetic mutations, and because, as immunologists have learned, the immune system has multiple layers of defense and offense. “You need really to combine, to synergize different modes of action,” says Özlem Türeci, a cancer immunotherapy pioneer who co-founded BioNTech, now known for collaborating with Pfizer on a COVID vaccine. “Different task forces with nonredundant, partially overlapping modes of action are combined. This is how the immune system has naturally evolved.”
Liquid Success
The dream of fighting cancer with the immune system dates back at least 125 years to William Coley of New York City, a physician who injected some of his cancer patients with bacteria in an effort to jump-start their body’s natural healing powers. Coley’s approach was taken up by a few other doctors. But it gradually fell out of favor after his death in 1936, to be replaced by advances in chemotherapy and, later, hormone and antibody treatments, which showed more consistent results in a greater number of patients.
The idea of boosting the immune system never entirely lost its appeal, though, in part because it was promoted by the Cancer Research Institute, a New York City–based philanthropy started in 1953 by Coley’s daughter. The field was not well respected for decades, Türeci says, but in more recent years, as HIV research has led to a deeper understanding of the immune system and genetics has enabled a more in-depth view of tumors, cancer investigators have stocked their arsenal with potent immunological weapons.
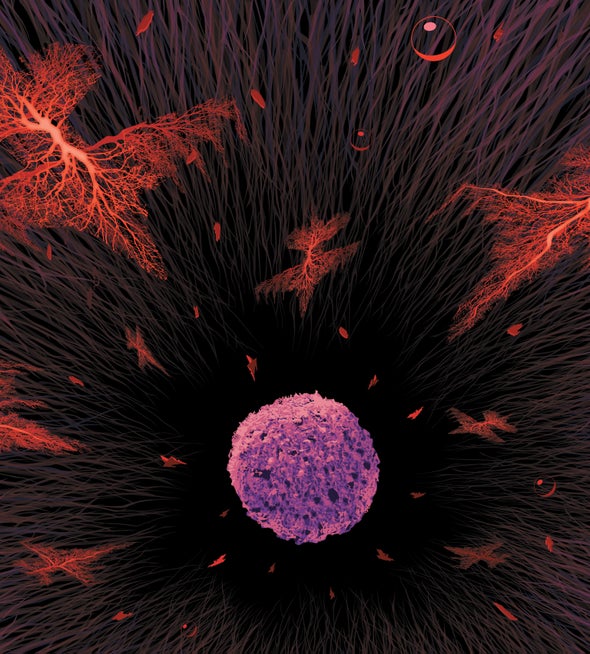
Among the most attractive targets for those weapons have been cancers of the circulatory and lymphatic systems such as leukemia and lymphoma. These diseases occur when various kinds of progenitor cells, called stem cells, that normally give rise to red and white blood cells (among other tissues) develop mutations and grow uncontrollably, crowding out healthy cells and robbing the body of their vital functions. Many of these so-called liquid tumors form when something goes wrong with a part of the immune system called B cells. Normally B cells generate antibodies against bacteria and viruses. (B cells also help to coordinate various other immune responses, along with another group of cells, T cells.) But when B cells become cancerous, they destroy the body from the inside out.
In the late 20th century investigators developed the biological equivalent of a guided missile that attached itself to a B cell protein (CD20) found on the cells’ surface at a specific, late stage of their existence. Dubbed rituximab, this monoclonal antibody signaled T cells to do something they do not usually do: attack and destroy these older, CD20-bearing B cells. CD20 is not a cancer-specific marker, though, and it appears on normal B cells as well as dangerous ones, so the drug killed both healthy and cancerous B cells. It turns out, however, that most people can live without B cells. (The same is not true of T cells, as the death of millions of people infected with T cell–targeting HIV tragically demonstrates.) And after the drug wore off, most patients eventually started making B cells on their own again from the stockpile of stem cells in their bone marrow. Clinical trials in the 1990s demonstrated that the combination of chemotherapy and rituximab was particularly effective against B cell–based cancers.

For Koehler, a retired special education teacher from Park Ridge, N.J., leukemia originated with mutant B cells, but rituximab made her very sick and seemed only partially effective, so she stopped taking it. In addition, tests indicated her cancer would resist standard chemotherapy. Because her malignancy was rapidly getting worse, her doctors suggested a then experimental immune treatment custom-designed to fight her form of leukemia. She agreed. The goal was to destroy all of Koehler’s B cells, as rituximab would, but with two key differences. A different protein on the B cells, CD19, was the mark. And rather than using a drug to paint a target on that protein, attracting killer T cells already in Koehler’s body, doctors took a more direct approach. They removed some of her T cells and genetically engineered them to attack CD19 without any prompting.
Investigators call these turbocharged cells chimeric antigen receptor T cells, or CAR Ts. They display some of the characteristics of both T cells and B cells in much the same way that ancient mythological creatures called chimeras were supposed to be made up of different animals. The U.S. Food and Drug Administration has approved a handful of CAR Ts so far, directed at CD19 or other cell surface markers. Previously CAR Ts had been used mostly as last-ditch therapies after others failed, but now they are being pushed earlier in the disease course, when patients—and their immune systems—are likely to be healthier and more responsive. Riddell says he is optimistic that improvements will come from treating patients earlier and perhaps from using combinations of CAR Ts designed to target both CD19 and CD20, as well as other antigens. He notes that among three recent trials in people with relapsed lymphoma, patients fared better if they received CAR Ts than the current standard-of-care bone marrow transplant.
Olson also volunteered for a CAR T trial long before the treatment was approved. One of the first three patients to sign up at the University of Pennsylvania for the experimental therapy in 2010, he saw it as his last chance to beat the chronic lymphocytic leukemia he had already lived with for 14 years. A few weeks after his infusion, he ended up in the hospital with flulike symptoms, one of three major side effects of the therapy. So many cancer cells were dying off so quickly that their removal was damaging his kidneys. After three days he stabilized, and his oncologist David Porter brought him some good news: already 19 percent of the T cells in his bone marrow consisted of the CD19-targeting CAR T cells. A month after the infusion they made up 100 percent of his T cells, and there was no sign of cancer left at all.
Olson says he has had no more side effects from the therapy, although his CAR T cells kept killing off his healthy B cells, so he needs monthly infusions of IVIG, antibodies that help fight off disease. In a study published in February 2022 in the journal Nature Medicine, researchers at Penn showed that some of his T cells and those of another patient treated around the same time, who has since died of COVID, still bore the CAR T signatures nearly a decade later and were able to kill leukemia cells in a lab dish. The CAR T cells that remained in Olson’s body had transformed from killer T cells into the more sentrylike CD4+ T cells. This suggests that patients like Olson have two distinct phases of response to CAR Ts: one in which killer T cells attack tumor cells and a second in which these CD4+ T cells maintain long-term remission by patrolling for any lingering cancer.
That evolution might not happen in everyone. Perhaps that is why Koehler’s remission did not lead to her being cured. By 2016, more than a year after a single infusion of CAR Ts derived from her own, altered cells, Koehler, then 59, was convinced she had hit the immunotherapy jackpot. Within a month of her treatment, scans showed no signs of cancer in her body. But she had already suffered through another of the potentially serious side effects of CAR Ts. The night she received her reengineered cells, a so-called cytokine storm landed her in intensive care. This reaction occurs when many more T cells than usual are activated at once, triggering a flood of chemical signals, called cytokines, that the immune system uses to communicate. The result can be a life-threatening frenzy of activity in which immune cells destroy healthy tissues, causing multiorgan failure. Riddell compares it to an explosion of inflammation inside the body. Koehler remained in intensive care for eight days, half of which she was in a coma and totally unresponsive. She has no memory of that time, but at one point, Koehler, an avid golfer, was so delusional that she asked nurses for help packing lunch for a pair of famous golfers.
By the time she got out of the hospital, in early March 2015, Koehler was incredibly weak but rebounding fast. A bone marrow test showed no evidence of cancer, and three weeks later she was back on the golf course. Koehler was one of the first clinical trial volunteers to endure this kind of dramatic, life-threatening cytokine storm. She says she was also the last of her doctor’s patients to end up in intensive care. Today when Koehler, a volunteer, counsels patients about to get CAR T therapy, she tells them they will stay in an apartment across the street from the hospital and might have to be admitted for a few days. But “no one really gets sick,” she says. “No one thinks they’re in Wyoming,” like she did during her delusions.
Another challenge with CAR T is its incredible price tag. The therapy routinely costs $375,000 to $475,000. Penn’s Carl June, in announcing the February 2022 Nature Medicine study Olson was part of, said the cost is high but less expensive than trying to keep someone alive on other, less effective therapies. Efforts are also underway to bring costs down. Until now, CAR Ts have been given mainly at academic medical centers after being manufactured in small research labs. But 140 biotechnology companies and every major pharmaceutical company, impressed by the therapy’s success, have gotten in on the act and should soon be producing the cells at larger scale for lower cost, based on improved manufacturing technologies and market competition, says Michel Sadelain, director of the center for cell engineering at Memorial Sloan Kettering Cancer Center in New York City.
Olson’s results suggest that few cell clones—just three make up the majority in his case—are long-lasting. If researchers can figure out what is special about those rare cells and just deliver those, instead of millions of others, the cost of therapy will drop substantially, Sadelain says. Researchers are also trying to develop cell therapy approaches that would be less personalized and more off the shelf but still effective, which could cost far less.
The other major challenge facing CAR T treatment is translating its success from liquid cancers to solid tumors—the kind that form lumps in breast, prostate, lung, skin and other tissues. CAR Ts may have a hard time leaving the bloodstream to find a solid tumor, Mellman explains. In the blood, the liquid tumor cells are relatively easy for the CAR Ts to locate. Even more important, CAR Ts for liquid cancers can be targeted specifically and safely to the affected cell lineages. There are no comparable cell lineages in solid tumors; they do not express surface molecules that are not also expressed by normal tissues. But Mellman sees tremendous long-term potential for this type of immune system manipulation. “What we’re looking at now with CAR Ts are still preliminary, almost crude approaches as compared to what I think will be possible when you can bring the full power of cell engineering to bear on the problem,” he says.
Solid State
Solid tumors pose other difficulties for immune treatments. They are often surrounded by a matrix of connective and other tissues, which blocks cells from entering the malignant mass. In addition, the internal pressure of a solid tumor is typically higher than that of its surroundings, which tends to flush out the chemical signals that the immune system uses to flag aberrant cells—not to mention many drugs.
Yet these tumors have shown some vulnerability. In 2011 the FDA approved a monoclonal antibody called ipilimumab to treat advanced cases of melanoma. Unlike traditional therapy, ipilimumab is not designed to kill tumors directly; rather it releases the biological brakes that some cancers are able to put on the immune system, freeing the body’s defenses to do a better job. (Carter was treated with a second-generation checkpoint inhibitor called pembrolizumab.)
Melanoma has a nasty habit of defrauding immune system cells. The clumps of cancer cells have an assortment of malformed proteins on their surface, which T cells are supposed to spot, swarm around and destroy before the aberrant growth has a chance to get any bigger. But every now and then a nascent tumor develops a way to send out chemical signals that tell the T cells all is well and to stand down.
In effect, the cancer cells have hijacked a normal feature of the immune system: a safety mechanism that tamps down the body’s rampaging defense cells before they start damaging healthy tissue. More specifically, this safety mechanism consists of a series of checkpoints, or gateways, that either rally defense cells to attack or turn them off, depending on which chemical signals are present. (If the checkpoints ever got stuck in the “open” position, the ensuing immune reaction would probably kill a person faster than any malignant growth could.)
Cancer cells have workarounds that enable them to hide from the immune system by disabling T cells that could kill them. Blocking that false signal with ipilimumab or other checkpoint inhibitors reawakens the immune cells, allowing them once again to zero in on their targets. Ipilimumab soon proved effective in lung cancer as well as melanoma, and pharmaceutical companies began developing other drugs that used the same strategy.
A 2015 study in the New England Journal of Medicine showed that more melanoma patients did better when given two checkpoint inhibitors instead of one. Still, doctors are not good at predicting who will respond to which checkpoint inhibitor or combination of treatments, so some patients have to keep experimenting with different therapies. Today about half the people treated with combination checkpoint inhibitors are alive for at least six years after their treatment. To confuse matters even more, some tumors that appear to attract few T cells still respond to checkpoint inhibitors, whereas the drugs sometimes have no effect on other tumors that contain lots of T cells—suggesting the cancer is playing other tricks.
That has made picking an effective solid tumor treatment for a particular individual a matter of trial and error, as Boyer’s experience shows. Two years after she had surgery to remove the cancerous mole from her back, Boyer learned that the melanoma had returned and was spreading throughout her lungs and chest. Because the growths were too large to be cut out, Boyer agreed, on the advice of her physicians, to take part in a clinical trial at the beginning of 2013 in which she would be injected with high doses of interleukin-2 (IL-2), one of dozens of different chemical signals that help to boost the immune system’s ability to fight cancer. At first the drug seemed to stop the growth of Boyer’s tumors, but after three months scans showed that the cancer was on the move again.
Boyer opted for a second clinical trial, this time pairing the recently approved checkpoint inhibitor ipilimumab with still another immune-signaling molecule known as IL-21. Within a few weeks, however, the side effects of the IL-21 treatment (nausea, diarrhea and unbearable pain) had become so disabling that Boyer had to stop getting the injections, although she continued receiving the ipilimumab. By the end of 2013 some of the cancerous spots had started to expand, so her medical team opted for radiation to try to limit the growth. By spring of the following year a few of these tumors were smaller, but new ones had appeared on her head and in her breast.
Surgery dispatched the lump in her breast, and two other immune-boosting therapies seemed to hold the rest of her tumors in check for a while. By January 2015, however, it had become clear that she needed another plan of action—new spots had begun to grow in her brain, breast and abdomen. A month later she entered a clinical trial that combined yet another checkpoint inhibitor with a drug that is supposed to slow tumor growth. Boyer’s cancerous spots remained stable for a while but eventually worsened.
The treatments battered Boyer’s body. By late 2016 she was spending her nights and many of her days in a plush loveseat to rest her back. During her sixth round of treatment, she was able to work most mornings in her job as a structural engineer. Otherwise she entertained herself by playing video games—Call of Duty was her favorite. She did not regret the game of Whac-A-Mole her doctors were playing with her cancer. “It seems to me that some of these treatments maybe slowed down the growth a little bit,” she said in 2016. One of her doctors, Boyer remembered, “said part of the game for melanoma was not necessarily finding the right treatment now but keeping yourself alive long enough until they find the right treatment.”
Unfortunately for Boyer, they didn’t. Her June 13, 2019, obituary notes that she had participated in clinical trials, “hoping to find treatments for future patients.” She was incredibly grateful for the outstanding medical care she had received at the Seattle Cancer Care Alliance and the University of Washington Medical Center, and she “wanted people to know that she was at peace with her death.”
Looking Ahead
Immunotherapy probably bought Boyer extra time. That is promising for cancer researchers, even if the ending was not fit for a fairy tale. Investigators no longer need to worry about whether their research will eventually help someone; now they can spend their time making effective treatments better. “We need to find the boundaries and limitations” and figure out how to work with the immune system to be more effective against a wider range of cancer types, Mellman says, but “this is an incredibly inspiring and thrilling way to do science.”
Eventually the process of selecting an immune treatment will become more logical, based on the characteristic immunological profile of a patient’s tumor, Mellman believes. A patient with a solid tumor will first have it biopsied to look for the presence of T cells. If enough T cells are in the tumor, the person will likely be given a single checkpoint inhibitor or maybe several inhibitors. (At present, the FDA has approved eight checkpoint inhibitors, with more under development.) If the tumor has not already attracted many T cells or if the T cells are unable to enter the tumor, scientists will have to find other approaches to generate, attract or facilitate the entry of tumor-specific T cells.
Researchers are also considering how to use standard cancer care, including radiation, targeted agents (such as mutant K-Ras inhibitors) and chemotherapy, to boost the immune response. Killing a number of tumor cells with lower doses of chemotherapy or radiation should release lots of cellular debris from the tumor, thereby alerting the immune system to send T cells to whatever abnormal growth remains. (Getting the balance right may be tricky because too much chemotherapy and radiation have also been shown to suppress parts of the immune system.) Then the addition of a checkpoint inhibitor might be able to effectively fight the weakened cancer before it has a chance to recover.
Other combinatory approaches may soon include cancer vaccines. Türeci’s BioNTech, among other companies, has been working on experimental vaccines that one day will be able to spur the immune system to attack cancer. So far BioNTech has made the best advances in treating colon cancer patients who have had surgery but are at high risk of recurrence and with personalized vaccines designed to attack an individual’s melanoma. Vaccines can trigger the body to generate a larger army of T cells, Türeci says, and then checkpoint inhibitors empower these T cells to roam freely in the body and attack lingering tumor cells.
Adding a vaccine might also help patients who got some response, like Boyer, but not a long-term benefit from a checkpoint inhibitor, Türeci says. Messenger RNA, the same vehicle used in BioNTech’s potent COVID vaccine, is a natural tool for immunotherapy, she adds. It amplifies the effect of the antigen by triggering a stronger immune response than earlier generations of cancer vaccines , which proved too weak. It is also viable for a personalized vaccine because one mRNA can easily be exchanged for another. “There is a new era for vaccines now,” she says.
Other researchers are manipulating T cell receptors, or TCRs, to encourage them to attack cancer cells, or using tumor-infiltrating lymphocytes, or TILs, which are taken out of the body, amplified in number in a lab and then reinfused. Steven Rosenberg of the National Institutes of Health has shown that about 15 to 20 percent of patients get a dramatic response from TILs, living as long as 15 years after treatment so far. “The question is, How do we make that a bigger pot?” Riddell asks.
Researchers are learning more about T cell exhaustion, a state in which the immune soldiers seem to just give up the fight. Single-cell sequencing is allowing insights at a more granular level than ever before. And gene editing is enabling scientists to put that new knowledge to good use, Riddell says. So new advances are bound to come. As he notes, it took 50 years to optimize chemotherapy, and checkpoint blockades and CAR Ts have been around for only a decade. “The potency of the immune system for eradicating cancers is really quite remarkable,” Riddell says. If cancer is a mountain range, “we’ve climbed the first peak, but there are more peaks.”
All these new therapies and combinations will be expensive, of course. The global market for oncology drugs is expected to top $250 billion a year by 2025, according to IQVIA, a health-care data company. Insurers and the public will not be willing or able to indefinitely combine drugs that can run to hundreds of thousands of dollars or more per patient. So companies are looking at manufacturing improvements, lower doses and shorter treatment times, among other approaches, to reduce treatment costs. But it is hard to argue with the value that more cures could provide.
Koehler, now 65, got six great years from her engineered T cells. Other than the IVIG infusions and regular checkups, she was able to lead a normal life. “I felt phenomenal,” she says. And it lasted so long that she “got a little cocky,” thinking her cancer days were over. But scans in late 2021 showed her leukemia had come roaring back. As of this writing, she was still waiting for her doctor to finish analyzing her blood work and recommend next steps.
“If we could do the CAR T again, I’d drive to the hospital right now,” she says. Doctors still have her cells, but CAR T is not yet approved for second-time use, and it is not clear whether her current cancer cells have the same CD19 receptors on their surface. Instead Koehler might end up on a drug called ibrutinib, an immunotherapy that is often given to treat chronic lymphocytic leukemia—but she would have to take it for the rest of her life. She told her doctor she would rather have another round of CAR T therapy: “I don’t want maintenance. I want you to knock it out again.” Cancer doctors hope immunotherapy will soon allow them to give many more patients extra years of high-quality life.