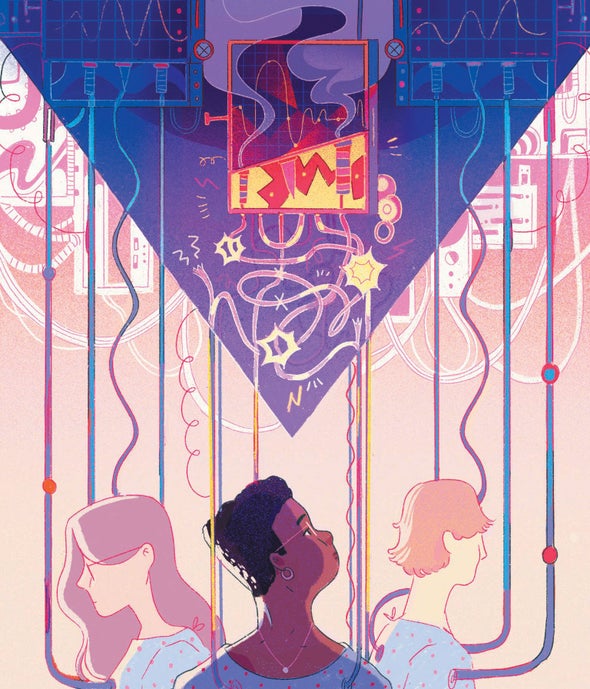
COVID has wreaked havoc on Black and Indigenous communities and other people of color, and U.S. medical institutions should be doing everything they can to root out and eliminate entrenched racial inequities. Yet many of the screening assessments used in health care are exacerbating racism in medicine, automatically and erroneously changing the scores given to people of color in ways that can deny them needed treatment.
These race-based scoring adjustments to evaluations are all too common in modern medicine, particularly in the U.S. To determine the chance of death for a patient with heart failure, for example, a physician following the American Heart Association’s guidelines would use factors such as age, heart rate and systolic blood pressure to calculate a risk score, which helps to determine treatment. But for reasons the AHA does not explain, the algorithm automatically adds three points to non-Black patients’ scores, making it seem as if Black people are at lower risk of dying from heart problems simply by virtue of their race. This is not true.
A paper published in 2020 in the New England Journal of Medicine presented 13 examples of such algorithms that use race as a factor. In every case, the race adjustment results in potential harm to patients who identify as nonwhite, with Black, Latinx, Asian and Native American people affected to various degrees by different calculations. These “corrections” are presumably based on the long-debunked premise that there are innate biological differences among races. This idea persists despite ample evidence that race—a social construct—is not a reliable proxy for genetics: Every racial group contains a lot of diversity in its genes. It is true that some populations are genetically predisposed to certain medical conditions—the BRCA mutations associated with breast cancer, for instance, occur more frequently among people of Ashkenazi Jewish heritage. But such examples are rare and do not apply to broad racial categories such as “Black” or “white.
The mistaken conflation of race and genetics is often compounded by outdated ideas that medical authorities (mostly white) have perpetuated about people of color. For example, one kidney test includes an adjustment for Black patients that can hinder accurate diagnosis. It gauges the estimated glomerular filtration rate (eGFR), which is calculated by measuring creatinine, a protein associated with muscle breakdown that is normally cleared by the kidneys. Black patients’ scores are automatically adjusted because of a now discredited theory that greater muscle mass “inherent” to Black people produces higher levels of the protein. This practice inflates the overall eGFR value, potentially disguising real kidney problems. The results can keep Black patients from getting essential treatment, including transplants. Citing these issues, medical student Naomi Nkinsi successfully pushed the University of Washington School of Medicine to abandon the eGFR race adjustment in 2020.
A 2019 study in Science examined an algorithm that is used throughout the U.S. health system to predict broad-based health risks. The researchers looked at one large hospital that used this algorithm and found that, based on individual medical records, white patients were actually healthier than Black patients with the same risk score. This is because the algorithm used health costs as a proxy for health needs —but systemic racial inequality means that health-care expenditures are higher for white people overall, so that the needs of Black people were being underestimated. In an analysis of these findings, sociologist Ruha Benjamin, who studies race, technology and medicine, observes that “today coded inequity is perpetuated precisely because those who design and adopt such tools are not thinking carefully about systemic racism.”
The algorithms that are harming people of color could easily be made more equitable, either by correcting the racially biased assumptions that inform them or by removing race as a factor altogether when it does not help with diagnosis or care. The same is true for devices such as the pulse oximeter, which is calibrated to white skin—a particularly dangerous situation in the COVID pandemic, where nonwhite patients are at higher risk of serious lung infections.
Leaders in medicine must prioritize these issues now to give fair and often lifesaving care to the people left most vulnerable by an inherently racist system.